Gene sequencing in the clinical laboratory – benefits and dilemmas
The ability to sequence genes in a cost-effective and efficient manner has provided the opportunity to offer whole exome and whole genome sequencing in the clinical laboratory setting. Whole exome sequencing (WES) provides sequencing data and identification of variations in the exons of an individual. The exons are the portions of genes that contribute to coding of proteins (Table 11,2). Whole genome sequencing (WGS) provides sequencing data on both introns and exons and identifies variations in almost all areas of the genome, including regions that may contribute to gene splicing or regulation.3,4 Both of these approaches have regions of the genome that are not well covered, so there is still missing information; however, a great majority of a person’s exome or genome can be sequenced, and numerous variations can be identified.
Click on table for larger image.
What might be the criteria to consider either of these tests? Both WES and WGS test ordering tends to be driven by the clinical phenotype of the individual.5 If someone presents with a recognized disorder or disease characterized by a well defined and limited number of mutations, then this approach is clearly overkill. But if an individual presents with a clinical phenotype that can have heterogeneous origins so that a number of genes may potentially contribute to the phenotype, then WES or WGS may be warranted. Likewise, if a disease or disorder is not well described or if the potential genetic origin is not yet known, then WES or WGS may be an option to attempt to identify the genetic cause or predilection of the patient’s issues.6,7
As one can imagine, identification of a given patient’s genetic variations via gene sequencing is merely the tip of the proverbial iceberg. Once the variations are identified one must determine for each variation if it has been reported previously and has a known consequence, if it has not been reported previously but would be likely to contribute to a clinical phenotype based on the type of mutation and the gene in which it resides, or if the significance of the mutation is completely unknown.
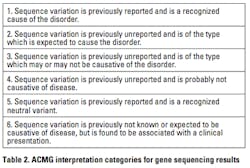
Determination of a known mutation can be accomplished by checking several key online resources that list gene mutations and the diseases or disorders they are known to cause or be in association with it. You may also identify a known variation that has previously been characterized as benign. If the variation is not reported previously, but is within a known gene, algorithms can be used to determine if the variation would be likely to impact gene integrity, expression/regulation, or function. If a clinical phenotype is inherited in a family, correlation of the presence of a given genetic variation in affected family members and not in unaffected family members may also provide evidence supporting the likelihood of the variation’s role in the phenotype. If these attempts to characterize the potential impact of a variation fail, then you are left with a variation of unknown clinical significance (VUS)—the black box of genetic sequencing.7,8 The various interpretations of mutations that can occur with WES and WGS have led to the definition of Interpretation Categories by the American College of Medical Genetics and Genomics (ACMG ) Laboratory Practice Committee Working Group8 (Table 2).
Acquiring knowledge of genetic variations from a test that was not ordered with the primary intent to obtain that information presents a dilemma. Although ultimately consent forms coupled with pre-test counseling will likely play a key role in which results to report from gene sequencing tests, there may be stratification of released results based on whether the disease is early- or late-onset and whether or not there are available medical actions to be taken.5,8,14,15 Disclosure of results from genetic sequencing is yet to be standardized and still under considerable debate.
In addition to determining whether unsolicited information on known genes should be disclosed, there is also the question regarding VUS. Should the patient and/or the physician have this information for potential future use? Mutation and disease correlations are being made at a fairly rapid pace. Who holds the burden of responsibility to repeatedly check the status of a given VUS? The laboratory? The physician? Or is it the patient’s responsibility to request it? There is clearly a cost associated with this continual review and if a new correlation is identified, there is the cost of the additional interpretation and subsequent report.16 Sophisticated laboratory information systems (LIS) could automate the complex re-analyzing and reporting to reduce costs; however, how would this be “ordered,” much less billed?17 There are many questions to be answered regarding the interpreting and reporting of gene sequencing results in a clinical laboratory.
Information on mutations or variations on many individuals could provide valuable research opportunities; however, this may require the need to closely follow a patient’s medical health throughout his or her life.18 Coordination of this effort—including databases to collect and programs to correlate the data—seems a bit daunting, but it could result in correlation of disease risk for common complex diseases like heart disease or diabetes or in correlation of reaction to medications or other therapeutic approaches. These correlations would support the practice of personalized medicine and assist in the maturation of pharmacogenomics.19-21
Gene sequencing is an extremely powerful tool, both in research and in the clinical laboratory. This tool also brings a multitude of social and ethical questions to the forefront, and these questions must be carefully considered and managed. Regardless, in your lifetime, you may very well find that you, your family, or a friend may be affected by gene-sequence testing.
Laurel Estabrooks, PhD, FACMG, is Vice President, Genetics Business Development, for SCC Soft Computer, provider of the SCC Genetics Information Systems Suite.
References
- Talking glossary of genetic terms. National Human Genome Research Institute website. http://www.genome.gov/Glossary/. Accessed August 20, 2012.
- MedTerms. Medicine Net website. http://www.medterms.com/script/main/hp.asp. Accessed August 20, 2012.
- ten Bosch JR, Grody WW. Keeping up with the Next Generation: Massively parallel sequencing in clinical diagnostics. JMD. 2008;10(6):484-492.
- Teer JK, Mullikin JC. Exome sequencing: the sweet spot before whole genomes. Hum Mol Genet. 2010;19(2):145-151.
- American College of Medical Genetics and Genomics (ACMG) Policy Statement: Points to consider in the clinical application of genomic sequencing. ACMG website. http://www.acmg.net/StaticContent/PPG/Clinical_Application_of_Genomic_Sequencing.pdf. Accessed August 20, 2012.
- Ku C, Naidoo N, Pawitan Y. Revisiting Mendelian disorders through exome sequencing. Hum Genet. 2011;129:351-370.
- Lander ES. Initial impact of the sequencing of the human genome. Nature. 2011;470:187-197.
- Richards CS, Bale S, Bellissimo DB, et al. ACMG recommendations for standards of interpretation and reporting of sequence variations: revisions 2007. Genet Med. 2008;10(4):294-300.
- Need AC, Shashi V, Hitomi Y, et al. Clinical application of exome sequencing in undiagnosed genetic conditions. J Med Genet. 2012:doi:10.1136/jmedgenet-2012-100819.
- Stranger BE, Stahl EA, Raj T. Progress and promise of genome-wide association studies for human complex trait genetics. Genetics. 2011;187:367-383.
- Mardis ER. Genome sequencing and cancer. Curr Opin Genet Dev. 2012;22:1-6.
- Oetting WS. Exome and genome analysis as a tool for disease identification and treatment: The 2011 Human Genome Variation Society Scientific Meeting. Hum Mutat. 2012;33(3):586-590.
- Gilissen C, Hoischen A, Brunner HG, Veltman JA. Unlocking Mendelian disease using exome sequencing. Genome Biol. 2011;12:228.
- Tabor HK, Stock J, Brazg T, et al. Informed consent for whole genome sequencing: a qualitative analysis of participant expectations and perceptions of risks, benefits, and harms. Am J Med Genet Part A. 2012;158A:1310-1319.
- Tabor HK, Berkman BE, Hull SC, Bamshad MJ. Genomics really gets personal: how exome and whole genome sequencing challenge the ethical framework of human genetics research. Am J Med Genet Part A. 2011;155(12):2916-2924.
- Sharp RR. Downsizing genomic medicine: approaching the ethical complexity of whole-genome sequencing by starting small. Genet Med. 2011;13:191-194.
- SoftMolecular® diagnostic molecular genetics laboratory system. SCC Soft Computer website. http://www.softcomputer.com/products-services/genetics/softmolecular/. Accessed August 20, 2012.
- Polychronakos C, Li Q. Understanding type 1 diabetes through genetics: advances and prospects. Nat Rev Genet. 2011;12:781-792.
- Mardis ER. Applying next-generation sequencing to pancreatic cancer treatment. Nat Rev Gastroenterol Hepatol. 2012;9:477-486.
- Pan S, Knowles JW. Exploring predisposition and treatment response – the promise of genomics. Prog Cardiovasc Dis. 2012;55(1):56-63.
- Wadelius M, Alfirevic A. Pharmocogenomics and personalized medicine: the plunge into next-generation sequencing. Genome Med. 2011;3(12):DOI:10.1186/gm294.