Clinical trial of remdesivir to treat COVID-19 begins
A randomized, controlled clinical trial to evaluate the safety and efficacy of the investigational antiviral remdesivir in hospitalized adults diagnosed with coronavirus disease 2019 (COVID-19) has begun at the University of Nebraska Medical Center (UNMC) in Omaha.
This is the first clinical trial in the United States to evaluate an experimental treatment for COVID-19, the respiratory disease first detected in December 2019 in Wuhan, Hubei Province, China. The regulatory sponsor of the trial is the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health.
The first trial participant is an American who was repatriated after being quarantined on the Diamond Princess cruise ship that docked in Yokohama, Japan, and volunteered to participate in the study. The study can be adapted to evaluate additional investigative treatments and to enroll participants at other sites in the U.S. and worldwide.
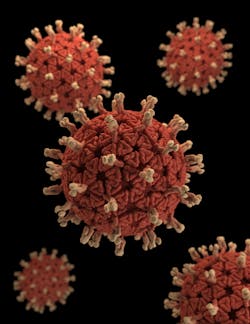
There are no specific therapeutics approved by the Food and Drug Administration (FDA) to treat people with COVID-19, the disease caused by the newly emergent SARS-CoV-2 virus (formerly known as 2019-nCoV). The Infection can cause mild to severe respiratory illness, and symptoms can include fever, cough and shortness of breath.
As of February 25, the World Health Organization (WHO) has reported approximately 81,000 confirmed cases of COVID-19 and almost 2,800 deaths in China, according to the Centers for Disease Control and Prevention (CDC).
Remdesivir, developed by Gilead Sciences Inc., is an investigational broad-spectrum antiviral treatment. It was previously tested in humans with Ebola virus disease and has shown promise in animal models for treating Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS), which are caused by other coronaviruses.
Clinical trials of remdesivir are also ongoing in China. NIAID developed the current study taking those designs into account, and in accordance with consultations convened by the WHO on the development of a therapeutic trial for patients with COVID-19.
Participants in the NIH-sponsored trial must have laboratory-confirmed SARS-CoV-2 infection and evidence of lung involvement, including rattling sounds when breathing (rales) with a need for supplemental oxygen or abnormal chest X-rays, or illness requiring mechanical ventilation. Individuals with confirmed infection who have mild, cold-like symptoms or no apparent symptoms will not be included in the study. In accordance with standard clinical research protocols, eligible patients will provide informed consent to participate in the trial.
All potential participants will undergo a baseline physical exam before receiving treatment. Eligible study participants will then be randomly assigned either to the investigational treatment group or the placebo group. The study is double-blind, meaning trial investigators and participants would not know who is receiving remdesivir or placebo. Participants in the investigational treatment group will receive 200 milligrams (mg) of remdesivir intravenously on the first day of enrollment to the study. They will receive another 100 mg each day for the duration of hospitalization, for up to 10 days total. The placebo group will receive, at an equal volume, a solution that resembles remdesivir but contains only inactive ingredients.
Clinicians will regularly monitor participants and will assign them daily scores based on a predefined scale of clinical outcomes that considers factors such as temperature, blood pressure and use of supplemental oxygen, among others. Participants also will be asked to provide blood samples and nose and throat swabs approximately every two days. Researchers will test these specimens for SARS-CoV-2.
Initially, investigators will compare participant outcomes on day 15 in both the remdesivir group and the placebo group to see if the investigational drug increased clinical benefit compared to placebo. Outcomes are scored on a seven-point scale ranging from fully recovered to death. Investigators will reevaluate this scale after reviewing data from the first 100 participants.
An independent data and safety monitoring board (DSMB) will monitor ongoing results to ensure patient well-being and safety as well as study integrity. The DSMB will recommend the study be halted if there is clear and substantial evidence of a treatment difference between drug and placebo.