Technology looks to support best outcomes in oncology testing for women
In the past few years, new technology advances and a focus on oncology testing have been hot topics in digital pathology, artificial intelligence (AI) and image analysis. In addition, cancer rates have been steadily increasing despite the breakthroughs in personalized medicine and treatment plans.
In 2019, over 268,000 new cases of breast cancer were diagnosed in women in the U.S. alone, and it is the second-leading cause of death among women. Similarly, ovarian cancer causes more deaths each year than any other gynecologic cancer in the U.S. These numbers are staggering and put a spotlight on the time, resources and dollars invested in research and development of technologies and methodologies to help reduce those numbers and improve the odds of survival for patients who are diagnosed with these, and other, cancers.
Focused areas of research
When it comes to breast and ovarian pathology, there are three main areas of focus for research and technology development:
- Developing the technology and the tools that support a faster time to diagnosis.
- Tools that will aid the pathologist in doing mundane, time-consuming tasks that a computer can do faster and with precision, such as calculations and identification of specific types of cells.
- Developing and determining the best applications for tools that better identify the specific types of cancer cells and other personal identifiers that will provide personal markers for better response to specific types of treatment. This will also quickly rule out treatments that will not have a positive or intended outcome.
Historically, breast cancer diagnosis begins with traditional scans such as ultrasound, mammography, MRI, PET, or CT scan. If a tumor or abnormal cells are detected, a biopsy is performed. There are different types of biopsy that are indicated based upon the original findings. They can be fine-needle aspiration, which uses a small needle; core needle biopsy, which uses a larger needle; MRI-guided biopsy; or surgical biopsy, in which all or part of a growth is removed and analyzed for cancer. Fine-needle aspiration and core needle biopsies may be performed using imaging, such as ultrasound, breast MRI, mammography, or CT scan.
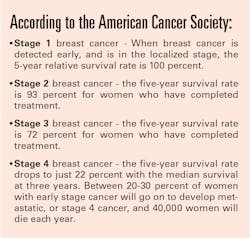
Once the sample has been taken, it is sent to the laboratory for interpretation and diagnosis. This process is crucial not only for a diagnosis, but also for the turnaround time for the diagnosis. The grading and determination of the specific type of tumor and cancerous cells dictates targeted therapy or other personalized treatments. These findings, and the speed of diagnosis, is what determines the best course of treatment for the patient and drives the best outcomes. The earlier cancer is detected, the earlier treatment can begin, and the better the outcome for the patient.Digital pathology and algorithms
Digital pathology speeds the time to diagnosis and provides pathologists with access to patient case information and whole slide images electronically and in an automated, integrated environment. This helps the pathologist by providing all the information they need to diagnose a patient quickly and accurately and enables the instantaneous distribution of that information back to the ordering clinician. Efficiency gains have been seen in the 20-40 percent range based upon studies done by labs that have implemented digital pathology.
There are artificial intelligence (AI) algorithms that can be integrated directly within the digital pathology workflow that provide the pathologist with rapid results. These results can identify and highlight items like breast cancer types – from triple-negative, inflammatory and metastatic to luminal, HER2-positive and more. There are algorithms that have been built for standard protocols – including ER/PR, Ki-67, HER2, P53, and PD-L1 – and there are algorithms that have been built for more esoteric or proprietary panels and assays.
Algorithms can also help with expeditiously locating regions of interest to aid pathologists by directing them to a specific area of the specimen, and can perform counts and calculations that determine the staging and grading of the tumor – all contributing to early and specific detection.
Ovarian cancer testing
Ovarian cancer testing is another area of focus for technological advancement. While it is the fifth-leading cause of death in women, it is very difficult to diagnose ovarian cancer early. There are three main types of ovarian tumors:
- Epithelial tumors: These tumors are the most common type of ovarian tumors and originate from cells that make up the outer surface (epithelium) of the ovaries.
- Germ cell tumors: These tumors originate from cells that produce eggs.
- Stromal tumors: These tumors originate from cells in the ovarian stroma. Stromal cells connect the parts of the ovary together and secrete female hormones.
Biopsy is also the method used to interpret cells and provide a diagnosis for ovarian cancer. It is the leading form of gynecological cancer in women. There are two methods of performing a biopsy for this form of cancer:
- Laparotomy - The surgeon cuts into the abdomen and examines the abdominal organs.
- Laparoscopy - The surgeon inserts a thin tube through a small cut in the abdomen. This procedure can be used to remove small benign cysts or ovarian cancer in its early stages. This method is also used to see if the cancer has metastasized into other areas.
There are also image analysis and AI algorithms that can identify specific biomarkers. Biomarkers indicate the presence (or potential for the presence) of a specific disease.
There are also biomarkers that can be indicated for therapeutic use in ovarian cancer. Digital pathology with integrated AI and image analysis algorithms can quickly identify these and bring them to the attention of the pathologist. There are some common biomarkers identified as being linked to different forms and functions in ovarian cancer:
- BRCA1 - hypermethylation of this gene is found in 10-15 percent of ovarian cancer cases.
- MLH1 - methylation of this gene’s promoter can be determined as indicative of the resistance to platinum-based treatments for epithelial ovarian cancer.
- HOXA9 - hypermethylation of this gene’s CpG promoter is found in cancer cells, including ovarian cancer.
The Institute of Cancer Research in London built an algorithm that looked for differences in tumor cell shapes. It found that a misshapen nuclei was indicative of a more aggressive form of ovarian cancer with a survival rate of only 15 percent over five years. This is another way that AI and image analysis can aid in a faster diagnosis, determination of specific cancer types and help provide a pathologist with information that is key to better outcomes. A computer program would be better able to quickly identify minor, almost imperceptible changes in shapes and highlight those for the pathologist to focus on.
Conclusion
Breast cancer is ranked first in new cancer diagnosis, and ovarian cancer is ranked as the sixth-highest for cause of death among all races, ethnicities and among both male and female.1 That is a scary figure considering that ovarian cancer is a major concern for half of the world’s population.
Given those statistics, it is understandable why the focus of technological advancements in pathology is on digital pathology, AI and image analysis as they support a faster diagnosis and increase accuracy when combined with the expertise of a pathologist. As digital pathology becomes more widely adopted, we can hope for faster diagnoses and more prevalent application of personalized, targeted treatment and better outcomes for the patient.
References:
- U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2019 submission data (1999-2017): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; June 2020 www.cdc.gov/cancer/dataviz. Accessed on July 31, 2020.
About the Author

Lisa-Jean Clifford
Lisa-Jean Clifford has been a noteworthy leader in the high-tech healthcare solutions space for more than two decades. Lisa-Jean’s passion for making a positive impact on the lives of patients through technology can be traced back to her tenure at McKesson and IDX, now GE Healthcare, where she served in vital business development and marketing roles, and to Psyche Systems, an LIS solution provider, where she was the CEO for eleven years. She is currently the President at Gestalt Diagnostics.
Now, recognized as an industry expert, she actively participates in numerous boards including the Association of Pathology Informatics where she serves as President and MLO’s Editorial Advisory Board. She is widely published in many top laboratory publications and noteworthy news sources, such as Forbes, CAPToday, Medical Laboratory Observer, and Health Data Management. Also, she is a highly sought-after speaker and focuses on delivering valuable content in critical areas such as lab automation including software and interoperability, digital pathology, AI in pathology, lab informatics, oncology, and women’s health.