Shortly after COVID-19 was declared a national emergency in the U.S., the Centers for Medicare & Medicaid Services (CMS) issued a memorandum on March 26, 2020, waiving the pre-pandemic requirement for remote sites to have a CLIA certificate when reviewing histopathology slides for primary diagnosis.1 The U.S. Food and Drug Administration (FDA) soon followed on April 24, 2020, with a guidance document relaxing enforcement policies that effectively allowed the interim use of digital pathology devices intended for “reviewing and reporting of digital pathology slides from remote locations” without a premarket notification submission.2 The guidance covered automated digital image microscopes, whole slide imaging (WSI) systems, image viewing and management software, and digital pathology displays — typically used in healthcare facilities, but also key components for reviewing and reporting of digital pathology slides from remote settings. The FDA cited continuity of patient care, reduction of healthcare personnel contact, and risk of exposure during the pandemic as the underlying rationale for its decision.
Over the past year and a half, these regulatory responses to the pandemic have brought to the foreground some of the benefits of digital pathology for clinical laboratories. For example, automated slide imaging can translate into faster, more accurate results and expedited clinical decision-making, resulting in better patient care. The reduction in manual labor required to handle and distribute slides for remote consultations improves process and cost efficiency. Importantly, digital pathology creates more possibilities for collaboration with colleagues at different locations, both in real time and asynchronously. This makes it much easier to invite second opinions and provide timely access to specialty expertise throughout the world, helping to ensure the highest standard of care.
Beyond operational advantages, digital pathology also holds promise for clinical decision support in a world where artificial intelligence (AI) and computational pathology are becoming increasingly useful and accepted tools within healthcare.
Developing and implementing a digital pathology strategy
When implemented properly, digital pathology has great potential to add value for a healthcare institution through data integration, cost efficiency, and improvements in quality and service. However, digital pathology implementation is complex, and, in most cases, full digitization across all operations and use cases cannot feasibly be achieved in a big bang approach. An important first step is to formulate a strategy based on current and future organizational needs, the regulatory environment, an assessment of resources — expertise, infrastructure, financial — and a vision for the outcome, including workflow metrics.
Defining digital pathology for your organization
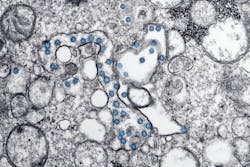
Digital pathology has different connotations for different enterprises. To create a manageable, scalable plan, begin by defining digital pathology for your organization and establishing a common vision for what it might encompass. Digital pathology, while oftentimes considered synonymous with whole slide imaging or slide scanning, may include other pathology imaging modalities, such as gross imaging, electron microscopy and telepathology. Determining which of these modalities are needed to best meet laboratory and organizational goals is an important first step. Even within a given modality, laboratories must decide which specific technologies and functions to implement in order to support intended and potential use cases. For example, WSI technology comprises not just the slide scanner, but also the software applications and server hardware to manage and display images, and in some cases, algorithms to assist the pathologist or technologist with image interpretation. There are no universally correct answers, and decisions should be based on your organization’s unique needs, goals, and expectations.
At this early stage, it is also important to determine where you will incorporate slide scanning into the laboratory workflow: before microscopic analysis, after sign-out but before archiving, on demand after archiving, or maybe a combination of these options? The right answer will vary according to specific circumstances.
A multidisciplinary team
Successful implementation of digital pathology will require many different types of expertise, including informatics, IT, quality, and clinical laboratory proficiency regarding the day-to-day operations of an anatomic pathology lab. Effective communication and change management skills are critical, as are input and buy-in from key stakeholders including pathologists, laboratory staff, administration and finance. A steering committee of representative stakeholders can drive the process of enlisting the right expertise.
Regulatory environment
Digital pathology is an emerging field, which means guidelines for clinical use will continue to evolve at local, state, and federal levels. A solid understanding of these requirements at all levels is key. Useful reference materials are available; one example is from the College of American Pathologists (CAP) Whole Slide Imaging Validation Guideline Expert Panel.3
Prioritizing initial use cases
The overall goal for implementation of digital pathology will drive selection of initial use cases. During the COVID-19 pandemic, the primary use case driving adoption of digital pathology has been routine WSI for the purposes of remote pathology. This is a logical starting point. If a scaled implementation of a specific use case (e.g., WSI) is preferred, one potentially effective strategy is to start with lower volume anatomic pathology services (e.g., autopsy, renal, transplant, pediatrics) to establish standard operating procedures and resolve preliminary issues, with the goal of onboarding higher volume services over time (e.g., genitourinary, gastrointestinal).
Starting with only WSI will make sense for some; others may choose to invest early in digitizing a broader range of imaging modalities. Other use cases (remote sign-out of intraoperative frozen sections, remote consultations and second opinions, tumor boards, image analysis) can also add value and be considered for early or future implementation. Alternatively, if a major goal is to improve clinical efficiency through the use of image analysis and/or artificial intelligence algorithms, a lab may want to consider the time required for various tasks in pathology to pinpoint where the greatest efficiency improvements are possible.
Infrastructure needs — now and for the future
The next step is building the required laboratory and IT infrastructure for digital pathology, which involves a range of functional considerations that should ultimately align with your defined use cases. Among the key elements of the infrastructure that you will need to evaluate are scanners, storage, and network speed.
A first consideration in evaluating scanners is throughput, with high throughput scanners outputting 60–100 slides per hour and allowing for continuous scanning at a 40x equivalent magnification. Scanners also differ by capacity, which refers to the number of slides an instrument can hold at once. For example, high-capacity scanners can batch anywhere from 100 to 1000 slides per batch. However, keep in mind that the greater a scanner’s batch capacity, the larger the physical footprint and capital investment will be for your laboratory. A third consideration is ease of use, or level of automation (e.g., automatic tissue detection) to enable lab staff to load slides and walk away. A final consideration is the extent to which a scanner will support positive patient identification. With barcoded slides and LIS interface/integration, lab staff can match slides to patient records with ease and accuracy. Ultimately, your specific digital pathology plan will guide your selection process for scanning technology that meets immediate needs and offers versatility to scale over time. Plans for more diverse use cases may require an assortment of scanners.
Then there is data storage. Expect your data storage needs to be higher than you originally anticipated. Current general estimates are 1.25 GB per slide at 40x equivalent magnification, doubled for system redundancy. Determine your initial storage needs, followed by the subsequent increases that will occur as you bring new services online. Starting small and building up allows you to detect and resolve issues with minimal impact on laboratory and digital pathology operations overall. Laboratories may reduce storage costs by selecting storage options appropriate for their needs. For example, a laboratory might include active and recently signed out cases in readily accessible but higher cost “hot” storage and then later move older cases for archiving using lower cost, but less rapidly accessed “cold” storage. Choose a data management strategy to meet your storage, security, maintenance, and networking needs.
Planning for the appropriate network speed also is important. Digital pathology consumes substantial bandwidth, typically requiring 1–10 gigabits per second (Gbps) with room for higher performance to support future growth. If the ideal network speeds are not available, discuss with your IT department the possibility of upgrading your network. Suboptimal network speeds will still allow some applications of digital pathology, but not all. For example, images can be downloaded locally or accessed from external storage media (e.g., flash drives) prior to review, obviating the need for fast network connections. Even if not ideal, such workarounds could still support uses as occasional second opinions.
Moving forward
As you identify your digital pathology strategy and key investment needs, an important final step is developing a comprehensive and realistic budget. It should take into account the costs of system components, including storage and networking, required to meet critical performance expectations, such as promised turnaround times and improvement goals. It is equally important to garner pathologists’ buy-in and earn their advocacy, starting early in the process and with the guidance of the steering committee. There is no universal path forward. Each organization will encounter its own challenges, pitfalls and burdens, but a clear, data-driven strategy for implementation will guide your organization into the future of digital pathology, with the potential to add value through data integration, cost savings, and improvements in quality and service.
References
- Centers for Medicare & Medicaid Services. (CMS). Clinical Laboratory Improvement Amendments (CLIA) Laboratory Guidance During COVID-19 Public Health Emergency https://www.cms.gov/medicareprovider-enrollment-and-certificationsurveycertificationgeninfopolicy-and-memos-states-and/clinical-laboratory-improvement-amendments-clia-laboratory-guidance-during-covid-19-public-health. Published March 26, 2020. Accessed September 21, 2021.
- U.S. Food and Drug Aministration. Enforcement Policy for Remote Digital Pathology Devices During the Coronavirus Disease 2019 (COVID-19) Public Health Emergency. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enforcement-policy-remote-digital-pathology-devices-during-coronavirus-disease-2019-covid-19-public. Published April 24, 2020. Accessed September 21, 2021.
- Validating whole slide imaging for diagnostic purposes in pathology. College of American Pathologists. https://www.cap.org/protocols-and-guidelines/cap-guidelines/current-cap-guidelines/validating-whole-slide-imaging-for-diagnostic-purposes-in-pathology. Accessed September 21, 2021.
About the Author

David McClintock, MD
is the Associate CMIO, Director of Digital Pathology, and Associate Director of Pathology Informatics at Michigan Medicine. He also is an Associate Professor of Pathology.