Platelets in the pipeline: Advancements in platelet technologies
Proper platelet function is an important component of many hemostatic disorders and a critical therapeutic target for cardiac and stroke prevention. Thus, a key objective of laboratory testing is to detect and understand the mechanisms of platelet dysfunction. The ability to diagnose platelet function deficiencies rapidly and accurately is vital to managing many bleeding conditions. Despite its importance, there are currently no tests available to assess platelet function in all situations. However, there are technologies in the pipeline that have potential for clinical adoption. The hope is that new strategies and technologies will expand platelet testing and antiplatelet therapy monitoring, while also providing improved turn-around-time, user-friendliness, reproducibility, and standardization.
Common platelet function tests aim to analyze a component of complicated platelet functions. While there are many instruments and systems available for measuring platelet function in the clinic, there are hurdles that make the task difficult. Problems include lack of standardization, time-sensitivity, dependence on fresh plasma, and highly technical hands-on time. These issues have driven variable results between clinical labs.1 In addition, mild bleeding disorders are difficult to diagnose due to subtleties in platelet dysfunction that may not be obvious or identifiable with current testing options using superphysiological conditions. Samples with thrombocytopenia have complex challenges that require careful data interpretation, especially when utilizing assays that require platelet-rich plasma (PRP). Most tests fail or provide aberrant data when using low platelet count samples. These challenges have stimulated the development of new platelet function devices and technologies to better meet the clinical needs of platelet function disorders and antiplatelet therapies.
Instrument additions offer fresh life to platelet function
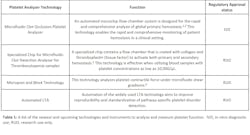
As platelet knowledge and technologies advance, so does the horizon of opportunities to improve platelet testing. From automation advancements for existing technology to expanding the scope of analysis, a platelet analyzer shake-up could be just around the corner (Figure 1).New FDA-cleared platelet analyzer—one test, one result
Platelet testing typically starts with a global primary hemostasis test to identify functional vs dysfunctional samples. A single test result is often unable to detect every cause of platelet dysfunction, thus multiple tests may be needed to determine a platelet function deficiency. To combat this, a newly cleared global testing system utilizing microfluidic clot occlusion with pressure sensing technology has arrived in the U.S. market (Table 1).2,3 This device fills the clinical need for global physiological testing parameters and empowers a single test result to detect primary hemostatic abnormalities or antiplatelet therapies. This technology has the potential to streamline global functional testing through the elimination of additional pathway-specific tests.
Lowering the thrombocytopenia roadblock
Most platelet function tests are sensitive to platelet counts, such that samples with low platelet counts may be problematic for the analytical abilities of platelet aggregometers and other assays.4 To address this, a specialized chip has been developed for microfluidic clot detection. It activates primary and secondary hemostasis in blood samples with platelet counts as low as 10,000/µL (Table 1).5 These chips contain a flow chamber that is coated with collagen and thromboplastin (tissue factor) through which blood flow mimics that typically seen in small arteries. As platelets become activated, platelet aggregation blocks channel flow, which increases flow pressure over time. This innovative technology may prove beneficial for analysis of hemostatic function in individuals with thrombocytopenia but is not approved for clinical use in the United States.
Platelet contractile force analysis
During primary hemostasis, platelets anchor to and aggregate at sites of vascular injury. Platelet contraction is the result of cell-signaling pathways that influence platelet shape, granule secretion, clot stiffness, and response to the stiffness of surrounding microenvironments.6,7,8 In essence, blood clots are dynamically active due to the contraction of platelets. Physiological alterations to the mechanical properties of blood clots are linked to bleeding, thrombosis, cancer, heart disease, and more.6 Platelet contraction is not currently measured nor approved for use in existing clinical assays but has potential to diagnose multiple types of platelet-driven deficiencies or dysfunctions.
New nanoscale technology has enabled the activity of platelet clumps and single platelets to be measured.6 The most advanced contraction measurement is with micropost and block technology which assesses platelet contractile forces under microfluidic shear gradients (Table 1).9 This technology could be used to better understand when platelet transfusions may be needed, titrate antiplatelet therapies, provide a global view of all steps of primary hemostasis, and characterize general clot formation and strength at various times. Collectively, careful analysis of platelet contractile forces provides insight into the biophysical outcomes of platelet function disorders.
Automated light transmission aggregometry
The gold standard for detecting pathway-specific platelet disorders has historically been automated light transmission aggregometry (LTA). LTA is flexible and can probe multiple platelet activation and aggregation pathways with various agonists in parallel.13 Despite these benefits, the LTA assay is manually intensive, time-consuming, is plagued by a lack of standardized laboratory practices, requires specialized technical training, equipment, and large sample volumes. To overcome the lack of standardization, new technology is in development to automate LTA (Table 1). Automated aggregometry could enable the ability to execute reproducible, gold standard platelet function testing without being dependent on specialized technicians. This automated instrumentation is being used in Europe but is not available in the U.S. market.Platelet product innovations—promising controls
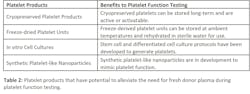
Platelet function testing frequently requires fresh donor plasma to serve as positive controls. Fresh donor plasma is a limited resource for many facilities and stands as a significant obstacle impeding the ability to provide platelet function services. To overcome the need for fresh donor plasma, cutting-edge blood product technologies are in development that may alleviate some of the related issues (Table 2).Cryopreserved platelet products (CPPs) offer the advantages of long-term storage coupled with platelet products that are active or activatable. Cryopreserved platelets are utilized in self-contained heparin induced thrombocytopenia (HIT) functional assays as alternatives to radioactive HIT functional assays.14 The ability of CPPs to control bleeding and blood loss during cardiopulmonary bypass surgery is also under investigation.15 Given that these platelet cryopreservation protocols produce active and functional platelets, it would be of great interest for future studies to assess the utility of CPPs as positive controls in platelet function assays.
An additional platelet product in the pipeline is freeze-dried platelets. Freeze-dried platelets are advantageous due to their ability to be stored at ambient temperatures for up to three years and can be rehydrated in sterile water to produce ready-to-use activated platelets.16 A phase 2 clinical trial is currently underway further investigating freeze-dried platelet units.17
In addition to purified platelet products from human plasma, platelets can be generated from various stem and differentiated cell cultures.18,19 Synthetic platelet-like nanoparticles are also being developed to mimic platelet hemostatic function to control bleeding.20 These proof-of-concept studies are promising, yet further developments are needed to meet clinical needs.
Utilization of these developing platelet products has the potential to eliminate the requirement of freshly drawn donor platelets for controlled platelet function testing. If effective, platelet function testing could become decentralized, technically simplified, and more accessible.
Conclusion
The recent boost of innovative technologies aims to fill the holes that are limiting accessible, accurate, and specific platelet function testing capabilities. The newly available clinical instruments and the up-and-coming platelet function tests are promising in being able to meet the clinical demands surrounding platelet function analysis. While most are still very much in the developmental pipeline, the future for better platelet testing options looks bright.
REFERENCES
1. Le Blanc J, Mullier F, Vayne C, Lordkipanidzé M. Advances in platelet function testing-light transmission aggregometry and beyond. J Clin Med. 2020;9(8):2636. Published 2020 Aug 13. doi:10.3390/jcm9082636.
2. Hosokawa K, Ohnishi T, Fukasawa M, et al. A microchip flow-chamber system for quantitative assessment of the platelet thrombus formation process. Microvasc Res. 2012;83(2):154-161. doi:10.1016/j.mvr.2011.11.007.
3. Hosokawa K, Ohnishi T, Kondo T, et al. A novel automated microchip flow-chamber system to quantitatively evaluate thrombus formation and antithrombotic agents under blood flow conditions. J Thromb Haemost. 2011;9(10):2029-2037. doi:10.1111/j.1538-7836.2011.04464.x.
4. Boknäs N, Macwan AS, Södergren AL, Ramström S. Platelet function testing at low platelet counts: When can you trust your analysis? Res Pract Thromb Haemost. 2019;3(2):285-290. Published 2019 Mar 19. doi:10.1002/rth2.12193.
5. Atari B, Ito T, Nagasato T, et al. A modified microchip-based flow chamber system for evaluating thrombogenicity in patients with thrombocytopenia. Thromb J. 2020;18(1):31. Published 2020 Oct 30. doi:10.1186/s12959-020-00244-9.
6. Williams EK, Oshinowo O, Ravindran A, Lam WA, Myers DR. Feeling the Force: Measurements of Platelet Contraction and Their Diagnostic Implications. Semin Thromb Hemost. 2019;45(3):285-296. doi:10.1055/s-0038-1676315.
7. Qiu Y, Brown AC, Myers DR, et al. Platelet mechanosensing of substrate stiffness during clot formation mediates adhesion, spreading, and activation. Proc Natl Acad Sci U S A. 2014;111(40):14430-14435. doi:10.1073/pnas.1322917111.
8. Kee MF, Myers DR, Sakurai Y, Lam WA, Qiu Y. Platelet mechanosensing of collagen matrices. PLoS One. 2015;10(4):e0126624. Published 2015 Apr 27. doi:10.1371/journal.pone.0126624.
9. Ting LH, Feghhi S, Taparia N, et al. Contractile forces in platelet aggregates under microfluidic shear gradients reflect platelet inhibition and bleeding risk. Nat Commun. 2019;10(1):1204. Published 2019 Mar 13. doi:10.1038/s41467-019-09150-9.
10. Lam WA, Chaudhuri O, Crow A, et al. Mechanics and contraction dynamics of single platelets and implications for clot stiffening. Nat Mater. 2011;10(1):61-66. doi:10.1038/nmat2903.
11. Schwarz Henriques S, Sandmann R, Strate A, Köster S. Force field evolution during human blood platelet activation. J Cell Sci. 2012;125(Pt 16):3914-3920. doi:10.1242/jcs.108126.
12. Myers DR, Qiu Y, Fay ME, et al. Single-platelet nanomechanics measured by high-throughput cytometry. Nat Mater. 2017;16(2):230-235. doi:10.1038/nmat4772.
13. Alessi MC, Sié P, Payrastre B. Strengths and weaknesses of light transmission aggregometry in diagnosing hereditary platelet function disorders. J Clin Med. 2020;9(3):763. Published 2020 Mar 12. doi:10.3390/jcm9030763.
14. Kanack AJ, Jones CG, Singh B, et al. Off-the-shelf cryopreserved platelets for the detection of HIT and VITT antibodies. Blood. 2022;140(25):2722-2729. doi:10.1182/blood.2022017283.
15. Cellphire Therapeutics, Inc., U.S. Army Medical Research and Development Command. Randomized Controlled Trial Comparing Dimethyl Sulfoxide Cryopreserved Platelets to Liquid Stored Platelets in Patients Undergoing Cardiopulmonary Bypass Surgery (CRYPTICS). clinicaltrials.gov. Published November 3, 2022.
16. Fitzpatrick GM, Cliff R, Tandon N. Thrombosomes: a platelet-derived hemostatic agent for control of noncompressible hemorrhage. Transfusion. 2013;53 Suppl 1:100S-106S. doi:10.1111/trf.12043.
17. Cellphire Therapeutics, Inc., Department of Health and Human Services. A Prospective, Multicenter, Randomized, Open-Label Phase 2, Parallel, Dose Ranging Multidose Study of Thrombosomes® vs Liquid Stored Platelets (LSP) in Bleeding Thrombocytopenic Patients. clinicaltrials.gov. Published October 31, 2022. Accessed January 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04631211?term=NCT04631211&draw=2&rank=1.
18. Reems JA, Pineault N, Sun S. In vitro megakaryocyte production and platelet biogenesis: state of the art. Transfus Med Rev. 2010;24(1):33-43. doi:10.1016/j.tmrv.2009.09.003.
19. Liu H, Liu J, Wang L, Zhu F. In vitro Generation of Megakaryocytes and Platelets. Front Cell Dev Biol. 2021;9:713434. Published 2021 Aug 12. doi:10.3389/fcell.2021.713434.
20. Anselmo AC, Modery-Pawlowski CL, Menegatti S, et al. Platelet-like nanoparticles: mimicking shape, flexibility, and surface biology of platelets to target vascular injuries. ACS Nano. 2014;8(11):11243-11253. doi:10.1021/nn503732m.
About the Author

Abigail Kasberg, PhD
is a Senior Support Scientist with DiaPharma Group. Abigail leverages her years of experience in scientific writing to carefully summarize published research findings and highlight the important roles of laboratory tests in clinical and research environments. Her analysis into the ever-expanding field of scientific discovery provides a streamlined understanding of how current and future diagnostic tests can better accommodate the unmet needs of laboratories.

Olivia Stricker, PhD
serves as the Commercial Business Development Manager of DiaPharma Group, a provider of platelet analyzers and hemostasis kits for clinical and research laboratories, including the TTAS-01 analyzer of total platelet function. She specializes in developing existing technologies for clinical use and spotting new technologies for commercialization.