CDC updates SARS-CoV-2 testing recommendations
The CDC says people, regardless of vaccination status, should be tested if they have symptoms of COVID-19. Asymptomatic healthcare personnel with a higher-risk exposure and patients or residents with prolonged close contact with someone with SARS-CoV-2 infection, regardless of vaccination status, should have a series of two viral tests for SARS-CoV-2 infection. In these situations, the CDC recommends testing immediately and 5-7 days after exposure.
In healthcare facilities with an outbreak of SARS-CoV-2, recommendations for viral testing healthcare personnel, residents, and patients (regardless of vaccination status) have not changed. In nursing homes with an outbreak of SARS-CoV-2, healthcare personnel and residents, regardless of vaccination status, should have a viral test every 3-7 days until no new cases are identified for 14 days.
The CDC also said hospitals and dialysis facilities with an outbreak of SARS-CoV-2 should follow current recommendations for viral testing of potentially exposed healthcare personnel and patients, regardless of vaccination status.
In nursing homes, unvaccinated healthcare personnel should continue expanded screening tests as previously recommended. At other healthcare facilities, however, fully vaccinated personnel who do not have a known exposure can be excluded from screening tests.
NGS test for prostate cancer and pre-treating aortic aneurysms
Researchers at the University of Michigan Rogel Cancer Center have developed a new urine-based, multi-biomarker test to detect aggressive prostate cancer that performed better than existing biomarker tests in initial preclinical evaluations.
The Urine Prostate Seq test, or UPSeq for short, uses next-generation genomic sequencing to analyze urine collected from men following a digital rectal exam.
The team used machine learning, a form of artificial intelligence, to zero in on 15 RNA transcripts that together create a “liquid biopsy” that outperformed the standard prostate-specific antigen blood test alone, a previous test developed at U-M called Michigan Prostate Score (MiPS) and several other existing biomarker tests, according to findings published in European Urology Oncology.
If a man is found to have an elevated PSA level, doctors first need to determine whether it’s a sign of prostate cancer, and if it is cancer, whether that cancer is aggressive. “The problem is that a patient can have multiple areas of cancer in the prostate and these areas may be different than each other,” explains senior study author Simpa Salami, MD, MPH, Assistant Professor of Urology at Michigan Medicine. “Because of this, both prostate biopsies and MRI scans can miss evidence of aggressive disease. So, this urine test is designed to tell us what’s really happening throughout the whole prostate.”
The research team believes the test has several potential clinical applications, including early detection of aggressive cancer in men at the time of an initial biopsy, and ruling out aggressive disease in men considering active surveillance – which involves monitoring their cancer through regular physical exams, blood tests, biopsies and imaging tests, and delaying treatment until the cancer shows signs of worsening.
A different University of Michigan study investigates a genetic culprit behind abdominal aortic aneurysm (AAA), a serious condition that puts people at risk of their aorta rupturing – a potentially deadly event.
For this study, a team of Michigan Medicine researchers investigated the role of an epigenetic enzyme called JMJD3 in the development of AAAs. They found the gene was turned on in people who had an AAA and that the gene promoted inflammation in monocyte/macrophages. When they blocked the enzyme, it prevented an aneurysm from forming.
“Targeting the JMJD3 pathway in a cell specific-manner offers the opportunity to limit AAA progression and rupture,” says lead author Frank Davis, MD, Vascular Surgery Resident at the Frankel Cardiovascular Center at Michigan Medicine.
“We are the first to perform an extensive single-cell RNA sequencing and gene expression analysis on human AAAs and non-aneurysmal aortic control samples,” Gallagher adds.
Software package enables deeper understanding of cancer immune responses
Researchers at the Bloomberg-Kimmel Institute for Cancer Immunotherapy at the Johns Hopkins Kimmel Cancer Center have developed DeepTCR, a software package that employs deep-learning algorithms to analyze T-cell receptor (TCR) sequencing data.
T-cell receptors are found on the surface of immune T cells. These receptors bind to certain antigens, or proteins, found on abnormal cells, such as cancer cells and cells infected with a virus or bacteria, to guide the T cells to attack and destroy the affected cells.
DeepTCR is a comprehensive deep-learning framework that includes both unsupervised and supervised deep learning models that can be applied at the sequence and sample level.
DeepTCR will enable investigators to study the function of the T-cell immune response in basic and clinical sciences by identifying the patterns in the receptors that confer the function of the T cell to recognize and kill pathological cells.
The software package, which employs a type of deep-learning architecture called a convolutional neural network, provides users the ability to find T-cell sequencing patterns that are relevant to a specific exposure, like a flu infection, a cancer or an autoimmune disease.
AMP urges caution in applying Ct values in clinical practice
The Association for Molecular Pathology (AMP) and the Infectious Diseases Society of America (IDSA) urge caution in the use of SARS-CoV-2 PCR cycle threshold (Ct) values for clinical decision-making.
“This all may change in the future based on expanded development and standardization of test methods and more robust clinical data, but at the current time, routine use of Ct values to inform clinical decisions is not advised,” said Blake W. Buchan, PhD, D(ABMM), who is a member the AMP Clinical Practice Committee (Infectious Diseases Subdivision) and Associate Professor in the Department of Pathology at the Medical College of Wisconsin.
He notes that current real-time PCR tests for SARS-CoV-2 are designed as qualitative assays that generate a binary result of “positive” or “negative.”
“Some of the tests also generate and report a cycle threshold (Ct) value, referring to the number of PCR cycles required to amplify the targeted viral nucleic acid to a detectable level, Buchan wrote. However, “there are no commercially available molecular tests for SARS-CoV-2 that have data supporting an indication to report quantitative results, including Ct values.”
Many factors could impact the precision of the Ct values, he said, such as the use of different specimen collection devices, specimen types, nucleic acid extraction methods, genomic targets, and RT-PCR chemistries.
“Reporting Ct values for public health or epidemiologic studies may be important to the continued research and understanding of SARS-CoV-2 infection and transmission dynamics. However, caution is urged in reporting these values formally into the medical record,” he wrote.
STDs at record high for 6th year in a row
The CDC reported a record high for sexually transmitted diseases (STDs) in 2019 for the sixth year in a row. Three most reported STDs were chlamydia, gonorrhea and syphilis, with nearly a 30% increase from 2015. Cases of syphilis among newborns nearly quadrupled.
In 2019, STD rates:
- For African American or Black people were 5-8 times that of non-Hispanic white people.
- For American Indian or Alaska Native and Native Hawaiian or Other Pacific Islander people were 3-5 times that of non-Hispanic White people.
- For Hispanic or Latino people were 1-2 times that of non-Hispanic white people.
The study also found that gay and bisexual men make up nearly half of all 2019 primary and secondary syphilis cases. It also found that young people 15–24 years old make up 61% of chlamydia cases and 42% of gonorrhea cases.
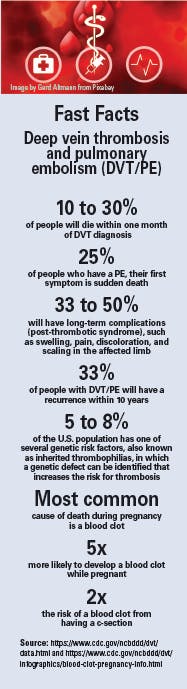
EMA finds possible links to blood clots with COVID-19 vaccines
The safety committee of the European Medicines Agency (EMA) concluded that unusual blood clots with low blood platelets should be listed as very rare side effects of Vaxzevria (formerly COVID-19 Vaccine AstraZeneca).
Separately, a Global Advisory Committee on Vaccine Safety from the World Health Organization (WHO) reviewed information from the EMA, the United Kingdom and others, concluding that “a causal relationship between the (AstraZeneca) vaccine and the occurrence of blood clots with low platelets is considered plausible but is not confirmed. Specialized studies are needed to fully understand the potential relationship between vaccination and possible risk factors.”
The EMA also said a warning about unusual blood clots with low blood platelets should be added to the product information for the COVID-19 vaccine from Janssen Pharmaceuticals. The committee concluded these events should be listed as very rare side effects of the vaccine. However, the EMA stressed that the overall benefits of the COVID-19 vaccine from Janssen outweigh the risks.
Johnson & Johnson said the company will resume shipments, as the rollout of the vaccine was temporarily paused in the United States.
The EMA committee took into consideration eight reports from the United States of serious cases of unusual blood clots associated with low levels of blood platelets, one of which had a fatal outcome. It reviewed 62 cases of cerebral venous sinus thrombosis and 24 cases of splanchnic vein thrombosis reported in the EU drug safety database (EudraVigilance), 18 of which were fatal.
All cases were people under 60 years of age within three weeks after vaccination, the majority in women. Specific risk factors have not been confirmed.
THE EMA’s committee noted that the blood clots occurred mostly at unusual sites, such as in veins in the brain (cerebral venous sinus thrombosis, CVST), the abdomen (splanchnic vein thrombosis) and in arteries, together with low levels of blood platelets and sometimes bleeding. The cases reviewed were very similar to the cases that occurred with the COVID-19 vaccine developed by AstraZeneca, Vaxzevria (previously COVID-19 Vaccine AstraZeneca).
One plausible explanation for the combination of blood clots and low blood platelets is an immune response, leading to a condition similar to one seen sometimes in patients treated with heparin, called heparin induced thrombocytopenia, HIT.