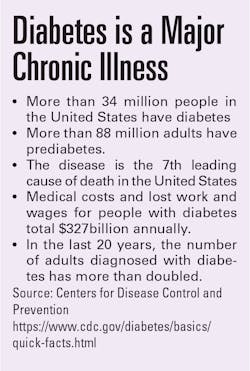
It also is an important test because diabetes is a major chronic condition. In 2018, 34.2 million Americans, or 1 in 10, had diabetes and 88 million American adults, or 1 in 3, had prediabetes, according to the Centers for Disease Control and Prevention (CDC). In addition, 7.3 million adults aged 18 years or older who met laboratory criteria for diabetes were not even aware that they had the disease.1
HbA1c tests measure the amount of HBA1c in red blood cells over the lifespan of those cells, or about 120 days. The test has numerous advantages over other methods. It does not require fasting or ingesting a concentrated glucose drink followed by a waiting period before testing. In addition, HbA1c can be measured multiple times per month, if necessary, making it ideal for not only diagnosing diabetes but also monitoring the disease.
Reversing an earlier position, the World Health Organization (WHO) recommended HbA1c as a diagnostic marker for diabetes in 2011 “provided that stringent quality assurance tests are in place and assays are standardized to criteria aligned to the international reference values, and there are no conditions present which preclude its accurate measurement.”2
The American Diabetes Association endorsed HbA1c testing in 2010.3
Relationship between HbA1c and age
However, there are some situations in which interpreting HbA1c test results should be approached cautiously, such as with older adults.
The concentration of HbA1c in blood increases as people age. The rates of diabetes and prediabetes also are higher in older age groups.
Among adults 18-44 years of age, 3% have been diagnosed with diabetes, compared with 12.4% of adults 45-64, 21.4% of adults 65-75, and 21.8% of adults 75 or older, according to an analysis by the Kaiser Family Foundation (KFF).4
Similarly, the CDC found that 24.3% of people 18-44 years old were diagnosed with prediabetes, increasing to 41.7% in people 45-64 years old, and 46.6% in people 65 years and older.5
Numerous researchers have examined the relationship between age and measures for diagnosing diabetes, such as HbA1c.
For example, a 2008 article in Diabetes Care found an association between HbA1c levels and age in patients without diabetes.6 The relationship held even after excluding study participants with impaired fasting glucose and impaired glucose tolerance. The analysis was based on information from 2,473 participants from the Framingham Offspring Study and 3,272 participants from the National Health and Nutrition Examination Survey (NHANES) 2001–2004 population.
A more recent study is described in a 2019 article in BMC Endocrine Disorders in which the authors confirmed an association between increasing HbA1c concentration in the blood and age in non-diabetic study participants. The relationship held up in lean, overweight, and obese study participants.7
However, official guidelines do not suggest different reference values based on age. (An HbA1c level of 6.5% is the currently established cutoff point for diagnosing diabetes.) The authors of the BMC study said that the one-size-fits-all reference value could impact the quality-of-care for patients. “Consequently, with respect to usage of a global cutoff for diagnosis of diabetes, disregarded age-related changes of HbA1c independent of disease might bear the risk of misdiagnosis in the elder population. Similarly, the HbA1c reference values for the monitoring of glycemia in patients with diabetes do not take the age of the individual into account potentially leading to unnecessary overtreatment with severe consequences,” the authors note.7
Prediabetes and the elderly
Another recent study focused on measures of prediabetes in the elderly.8 The cohort study followed 3,412 older adults without diabetes living in a community setting for 6.5 years. The mean age was 75.6 years and included both frail and non-frail older adults.
During the study period, 1,490 participants, or 44%, met the definition of prediabetes, with HbA1c levels of 5.7% to 6.4%, while 1,996, or 59%, met the criteria for prediabetes with fasting glucose levels (FGLs) of 100-125 mg/dL. A total of 1,004, or 29%, met both the HbA1c and IFG criteria.8
By the end of the study period, however, few of the participants with prediabetes had become diabetic. Among those who met the criteria for prediabetes by HbA1c concentrations, 97, or 9%, progressed to diabetes and 148, or 13%, lowered their glycemia levels to a normal level. Of those with IFG at baseline, 112 (8%) progressed to diabetes and 647 (44%) achieved normal glycemia levels.8
The authors said the findings suggest that these measures of prediabetes may not be meaningful for guiding patient care in older adults.
Reasons for the relationship
What is the reason behind the relationship between age and HbA1c?
One of the studies she points to was described in a 1993 article in Clinica Chimica Acta on the acceleration of hemoglobin glycation with aging.9
Meanwhile, a 2017 study conducted in China showed that the relevance of HbA1c as a measure for diabetes decreased with age, which the authors said happens because of decreases in red blood cell (RBC) counts as people age. But how this occurs is unclear, the authors said.10
However, they speculated about how decreasing RBC counts could impact HbA1c as a diagnostic test. They wrote, “We put forward two possible explanations. First, the decreased RBC count caused by the decreased cell turnover could result in the increased RBC lifespan with aging, increasing the levels of HbA1c. Second, previous studies have reported that the cellular damage caused by aging, including altered enzyme activity, decreased membrane lipids and increased cell fragility, promoting the acceleration of hemoglobin glycation. Under these conditions, the HbA1c level could not truly reflect the average blood glucose concentration in the elderly, resulting in the decreased diagnostic efficiency with aging.”8
Advice for diagnosis and clinical practice
All of this information begs the question: How should HbA1c results be interpreted in older adults, and what does this mean for clinical practice?
Sivaraman said, “Since the data available today on the effect of age on A1c levels is limited, laboratories need to exercise caution when using A1c as a sole diagnostic marker in the elderly. It is important to look at the individual’s history and complement the A1c with other tests that can help arrive at a robust diagnosis. Attention needs to be paid specifically to individuals who flank the decision-making point wherein age could possibly play a role in the change in diagnosis as the individual ages.”
Authors of the 2019 article in BMC Endocrine Disorders focusing on the relationship between HbA1c and age suggested age-stratified reference ranges for Caucasians. For people aged 20-39 years, the authors propose an upper reference limit for HbA1c of 6.0%, compared with 6.1% for people 40-59 years, and 6.5% for people who are 60 years or older.
In a podcast interview with JAMA Internal Medicine, Elizabeth Selvin, PhD, Professor of Epidemiology at Johns Hopkins Bloomberg School of Public Health and an author of the prediabetes study, suggested how to respond to HbA1c test results indicating prediabetes in elderly patients. “I think we need to rethink definitions of prediabetes in older adults,” Selvin said. “They simply don’t have the same prognostic meaning as they have in younger individuals.11
Rather than focusing on a diagnosis of prediabetes, Selvin recommends that clinicians counsel their older patients about the broad health benefits of a healthy lifestyle, including eating healthy food, reducing consumption of processed foods, quitting smoking, and getting regular exercise, such as walking or lifting weights. 11
However, she emphasized that prediabetes is still an important concept overall. “Identifying people prior to the onset of diabetes, especially in middle age, is really critical. Preventing the onset of diabetes can then help us prevent the onset of major complications.” 11
References
- Centers for Disease Control and Prevention. National diabetes statistics report, 2020. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed October 31, 2022.
- World Health Organization. Use of glycated Haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: Abbreviated report of a WHO consultation. https://www.who.int/diabetes/publications/report-hba1c_2011.pdf. Published 2011. Accessed January 5, 2022.
- Standards of medical care in diabetes—2010. American Diabetes Association. 2010 Jan;33 Suppl 1(Suppl 1):S11-61. doi: 10.2337/dc10-S011.
- Percentage of adults with diagnosed diabetes by age group. Kaiser Family Foundation. https://www.kff.org/other/state-indicator/adults-with-diabetes-by-age/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed January 7, 2022.
- Centers for Disease Control and Prevention. Prevalence of prediabetes among adults. https://www.cdc.gov/diabetes/data/statistics-report/prevalence-of-prediabetes.html. Updated June 30, 2020. Accessed January 7, 2022.
- Pani L, Korenda M, Meigs, J, Driver C, et al. Effect of aging on A1C levels in individuals without diabetes: Evidence from the Framingham Offspring Study and the National Health and Nutrition Examination Survey 2001–2004. Diabetes Care. 2008;31(10):1991–1996. doi.org/10.2337/dc08-0577.
- Masuch A, Friedrich N, Roth J, Nauck M, et al. Preventing misdiagnosis of diabetes in the elderly: age-dependent HbA1c reference intervals derived from two population-based study cohorts. BMC Endocr Disord. 2019.19, 20. doi.org/10.1186/s12902-019-0338-7.
- Rooney M, Rawlings A, Pankow J. Risk of progression to diabetes among older adults with prediabetes. JAMA Intern Med. 2021;181(4):511-519. doi:10.1001/jamainternmed.2020.8774.
- Nakashima K, Nishizaki O, Andoh Y. Acceleration of hemoglobin glycation with aging. Clin Chim Acta. 1993 Apr 16;215(1):111-8. doi: 10.1016/0009-8981(93)90254-2.
- Wu M, Lin H, Gao J, et al. Effect of age on the diagnostic efficiency of HbA1c for diabetes in a Chinese middle-aged and elderly population: The Shanghai Changfeng Study. PLoS One. 2017 Sep 8;12(9):e0184607. doi: 10.1371/journal.pone.0184607.
- Risk of progression to diabetes among older adults with prediabetes. JN Learning. JAMA Internal Medicine. Podcast. https://edhub.ama-assn.org/jn-learning/audio-player/18583887. Posted February 8, 2021. Accessed January 7, 2022.