Body fluid cellular analysis is used by physicians to get substantial information regarding a patient’s medical conditions, including inflammatory diseases, infection, hemorrhage and malignancy.1 Traditionally, body fluid analysis is performed manually with an optical microscopy, which is considered the gold-standard method for cell counting.2 However, manual counting is time-consuming, labor intensive, and subject to high inter-observer variability and potential poor reproducibility.3 The burden of body fluids analysis is only increased with the high pressure, low resource environment we live in today.
The challenge for laboratories
Laboratories and healthcare systems across the world have been placed under sustained pressure during the COVID-19 pandemic.4 This is exacerbated by the shortage of labor. In fact, according to Medical Laboratory Observer’s 2021 annual salary survey of laboratory professionals, 80% of respondents noted shortages having a “moderate to large impact” on operational efficiency.5 The challenge of labor shortages cannot be overcome easily as between 2007 and 2017, the number of active pathologists in the U.S. decreased by approximately 17.5%, a trend that has continued.6 This dramatic lack of supply and demand equilibrium demands laboratories to do more with less, and this is where automation has a role to play — to help to reconcile this in equilibrium and deliver high-quality results.
Despite wage growth, the labor force participation rate remains near its lowest level since the 1970s. In the face of this shortage, hospitals are turning to automation.7 Automated methods for body fluid cell counts have been rapidly replacing manual hemacytometer methods, while technological advances in hardware and software engineering have developed instruments with expanded analytical capabilities that enable processing multiple specimen types including urine, cerebrospinal fluid (CSF), peritoneal fluid, pleural fluid, synovial fluid, and lavages on a single analyzer.8
High quality body fluid analysis
Although electronic cell counters are available, they are usually ineffective for CSF and other body fluids owing in part to elevated background counts and other interference that can falsely elevate low cell counts.9,10
The introduction of automated methods of analysis has reduced inter-operator variability and improved turnaround time and precision,11 and many automatic analyzers have emerged in recent years, offering improved accuracy, efficiency, and standardization,12 as well as rapid, reliable, and accurate counting of red blood cells (RBCs) and WBCs (differential) in cerebrospinal and other body fluids.13 Beyond precision and reliability, automation can also provide insight for probable detection of multiple parameters, even in scant amounts, that could have been missed on manual analysis, like presence of yeast like cells, crystals, small round cells and others.14
Lower costs and labor for urinalysis
A clinical study that was done with an automated urinalysis analyzer in Spain that included a body fluid module showed that the comparison of annual costs for current practice versus the automated examination of urine samples found average cost savings of €340,003 per year. Assessment of body fluids using the automated analysis system would provide average annual savings of €1063. The use of automation would save 1,615 hours annually for laboratory personnel.15
Faster TAT for body fluid analysis
Manual screening of a urine specimen takes up to six minutes per sample while an automated system generates the result in around one minute.14 This dramatically impacts turnaround time. Salem Hospital Regional Laboratory conducted a study to compare the number of tests that are resulted at 30, 45, and 60 minutes. The hospital found an improvement of 30% at 30 minutes, 9% at 45 minutes, and 3.2% at 60 minutes. The urinalysis staff also handled hematology duties, and the post-implementation improvement for CBCs was 44% at 30 minutes, 22% at 45 minutes, and 8% at 60 minutes.16 In another hospital, automation helped to improve turnaround time with 92% of urines reported in 30 minutes from the time the laboratory received them.17
How to automate
There are several ways to automate body fluid analysis:18
- Method 1. Enhanced impedance counting is available on some hematology platforms and relies on the displacement of electrical field to provide information on particle size and volume. This aids in classifying particles.
- Method 2. Simple flow cytometry measures cell granularity, size, and light scatter. This can be performed on some hematology platforms. The laser detects size, volume and shape, which aides in classifying particles.
- Method 3. Particle and image recognition is a method in which the cells are counted by digital flow morphology, allowing the system to capture actual images of particles and classify them by size, shape, contrast, and texture. A visual inspection by a technician can be done after an analysis is complete if they need to identify real cells from artifacts.
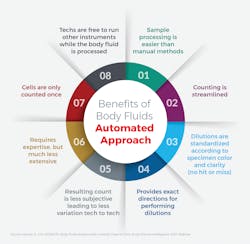
Regardless of the methodology used, the benefits of automation are clear, and for laboratories, the most important one is that of lightening the load. And while modern urine analyzers have reduced some of the burden associated with manual body-fluid analysis, new innovations in body fluid analysis deliver faster speed to results and significant improvement in laboratory efficiencies.
References
- Fleming C, Russcher H, Lindemans J, de Jonge R. Clinical relevance and contemporary methods for counting blood cells in body fluids suspected of inflammatory disease. Clin Chem Lab Med. 2015;53:1689–1706. doi: 10.1515/cclm-2014-1247.
- Alcaide Martín, María José, Altimira Queral, Laura, Sahuquillo Frías, Laura, Valiña Amado, Laura, Merino, Anna and García de Guadiana-Romualdo, Luis. Automated cell count in body fluids: a review. Advances in Laboratory Medicine / Avances en Medicina de Laboratorio, vol. 2, no. 2, 2021, pp. 149-161. https://doi.org/10.1515/almed-2021-0011.
- Cho, Jooyoung et al. Performance evaluation of body fluid cellular analysis using the Beckman Coulter UniCel DxH 800, Sysmex XN-350, and UF-5000 automated cellular analyzers. Ann Lab Med. 2020 Mar;40(2):122-130. doi: 10.3343/alm.2020.40.2.122.
- Aisyah, Dewi N. et al. Laboratory readiness and response for SARS-CoV-2 in Indonesia. Front Public Health. 2021; 9:705031. doi: 10.3389/fpubh.2021.705031. Print.
- Nadeau K. MLO’s 2021 annual salary survey of laboratory professionals. Medical Laboratory Observer. mlo-online.com/management/careers/article/21210806/mlos-2021-annual-salary-survey-of-laboratory-professionals Published February 22, 2021. Accessed December1, 2021.
- Metter DM, Colgan TJ, Leung ST, Timmons CF, Park JY. Trends in the US and Canadian pathologist workforces from 2007 to 2017. JAMA Netw Open. 2019;2(5):e194337. doi:10.1001/jamanetworkopen.2019.4337.
- To solve labor shortage, companies turn to automation. Wall Street Journal. https://www.wsj.com/podcasts/the-journal/to-solve-labor-shortage-companies-turn-to-automation/11a31603-b66a-438c-a372-791b848436b5. Published October 22, 2021. Accessed December 1, 2021.
- Scott G. An automated approach to body fluid analysis. Medical Laboratory Observer. https://www.mlo-online.com/home/article/13006695/an-automated-approach-to-body-fluid-analysis. June 2014.
- Strasinger SK, Di Lorenzo MS . Cerebrospinal fluid. In: Urinalysis and Body Fluids. 4th ed. Philadelphia, PA: FA Davis; 2001:149–168.
- Aune MW, Becker JL . Automated flow cytometric analysis of blood cells in cerebrospinal fluid. Am J Clin Pathol. 2004;121:690–700. doi: 10.1309/EKFW-9E3L-LFXE-15X9.
- Danise P, Maconi M, Rovetti A, Avino D, Di Palma A, Gerardo Pirofalo M, Esposito C. Cell counting of body fluids: comparison between three automated haematology analysers and the manual microscope method. Int J Lab Hematol. 2013;35(6):608-13. doi: 10.1111/ijlh.12093. Epub 2013 May 6. PMID: 23647736.
- Sandhaus LM. Body fluid cell counts by automated methods. Clin Lab Med. 2015 Mar;35(1):93-103. doi: 10.1016/j.cll.2014.10.003. Epub 2014 Dec 4. PMID: 25676374.
- Koo MS, Lim J, Kim SY, Koo SH, Kwon GC. Comparison of red blood cell, white blood cell and differential counts between UF-5000 system and manual method. J Lab Med Qual Assur. 2019;41:172-178. doi.org/10.15263/jlmqa.2019.41.3.172.
- Bargotya M, Kumar L, Das P, Kachhap P, Sachdeva V and Monika K. Evaluation of advantages of multiple parameters of an automated urine analyzer in clinical practice. SciMedCentral. https://www.jscimedcentral.com/ClinicalCytology/clinicalcytology-4-1110.pdf. Published 2018. Accessed December 1, 2021.
- Herráez Carrera, Óscar, and María Del Monte Jarabo Bueno. Cost Analysis of the Automated Examination of Urine with the Sysmex UN-Series in a Spanish Population.” PharmacoEconomics - Open. 2020;4(4): 605-613. doi:10.1007/s41669-020-00200-3.
- Paxton A. Unexpected findings. CAP Today. https://captodayonline.com/Archives/feature_stories/0707UrineSide2.html. Published July 2007. Accessed December 1, 2021.
- Paxton A. Automation nudges urinalysis into spotlight. CAP Today. https://captodayonline.com/Archives/feature_stories/0707Urine.html. Published July 2007. Accessed December 1, 2021.
- Body fluids analysis with linearity down to zero. Beckman Coulter. https://www.beckmancoulter.com/en/blog/diagnostics/body-fluids-analysis. Published May 7, 2021. Accessed December 1, 2021.
About the Author

Matt Rhyner, PhD, MBA
is Vice President and General Manager of Urinalysis at Beckman Coulter Diagnostics.