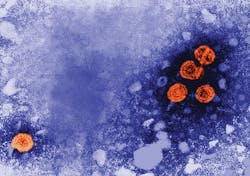
Worldwide, hundreds of millions of people are living with chronic viral infections that, when left untreated, claim the lives of millions every year. Among the biggest killers are HIV, hepatitis B (HBV), and hepatitis C (HCV). The World Health Organization (WHO) estimates that there are 36.7 million HIV, 257 million HBV, and 71 million HCV chronic infections.1-3
HIV: a (partial) success story
The United Nations has set an ambitious goal of “90:90:90” to tackle the HIV epidemic: By 2020, 90 percent of people living with HIV will be diagnosed; 90 percent of those diagnosed will be linked to care; and 90 percent of those linked to care will have achieved viral suppression.4 This policy and the actions it has driven have had a dramatic impact on the HIV epidemic. While one million people a year die from HIV-associated illness, mortality associated with the disease is in decline for the first time since the emergence of HIV.1
The role of diagnostics in turning this tide cannot be overestimated, as diagnostic testing is integral to the first and last of “90’s.” Since the first HIV tests became available more than 30 years ago, advances have been made to help detect HIV at every stage of the continuum of care. Once HIV has been diagnosed, it is valuable to assess potential antiretroviral drug resistance using an FDA-approved HIV resistance test so therapy can be optimized and to prevent the development of further drug resistance that might compromise future treatment options. In addition, the degree of viral suppression is determined by measuring the level of viral RNA present in the patient’s peripheral blood (known as the viral load). The excellent progress made in diagnostic and drug development as well as implementation science in the fight against HIV makes it possible to think that an AIDS-free generation may be achievable in the foreseeable future.
Hepatitis: setting a goal
In contrast to the declining mortality rate associated with HIV, the number of people dying of liver disease related to viral hepatitis infection among the estimated 328 million people with chronic hepatitis B or C infections worldwide has increased to 1.4 million per year. Unless more is done to tackle the problem, the number will continue to increase due to the progressive nature of the disease.2,3,5 The WHO has taken a bold step by setting the goal of eliminating viral hepatitis as a public health problem by 2030. This goal involves reducing the annual number of new cases by 90 percent and the number of deaths related to viral hepatitis by 65 percent by that year.5 Achieving that is possible, in large part due to the development of new therapies for the treatment of HCV that have achieved cure rates reportedly as high as 100 percent in clinical trials and 94 percent to 98 percent in real-world studies.6,7
The amazing success of new therapies for HCV will have little or no impact on the epidemic, however, unless the millions of people unknowingly living with an active infection are identified so they can be treated. Like HIV diagnosis, HCV diagnosis relies heavily on screening for the presence of antibodies produced by the body in response to the infection. In contrast to HIV-1 infection, approximately 25 percent of people infected with HCV can spontaneously resolve (cure) the infection without treatment.8 This means that diagnosis of an active HCV infection involves a two-phased diagnostic approach: first, detection of antibodies to HCV; and second, confirmation of active infection with a test that detects the actual presence of viral nucleic acid, such as an HCV viral load or protein such as HCV antigen. One drawback of screening for antibodies to HCV is a potential delay in diagnosis of the infection, since HCV seroconversion (the point when antibodies to HCV are detectable) may occur several weeks to months after virus exposure. This “seroconversion window” is defined as the time interval from infection to detection of antibodies to HCV.9 The window period was narrowed from up to 13 weeks with EIA-based testing to 1.34 days with nucleic acid-based assessment.10
The latest HCV diagnostics
Diagnostics manufacturers are continually improving the sensitivity of serology tests to obtain results closer to HCV RNA or HCV core antigen and narrow the seroconversion window. Current anti-HCV tests have narrowed the window period to six to eight weeks. In 2016, the WHO and the European Association for the Study of the Liver (EASL) both incorporated into their guidelines HCV core antigen testing as an alternate to HCV RNA for the confirmation of active infection. HCV core antigen is significantly less expensive and less complex than HCV RNA, allowing for simplification and increased access to HCV diagnostics.11,12 This development is important, as many of the 71 million people with chronic HCV infection live in low- to middle-income countries or are part of marginalized populations such as people who inject drugs or sex workers (or gay men and women in countries where homosexual behavior is stigmatized or criminalized).3 EASL also incorporated HCV core antigen testing to monitor patients’ response to therapy and determination of sustained virologic response (“cure”), further simplifying and driving down the overall cost of treating HCV infection.12
Current diagnostic tests require phlebotomy followed by refrigeration or freezing of the sample until the time of testing. This limits implementation of HCV diagnosis and initiation of therapy in resource-limited settings where venipuncture and cold chain transportation may not be available. The use of specimen types other than refrigerated or frozen blood products for HCV diagnostic assays may eliminate this logistical limitation and improve clinical management of patients.13 In resource-limited settings, the collection of dried blood spots (DBS) represents an alternative which is minimally invasive, does not require a trained phlebotomist, and has proven effective in the diagnosis and monitoring of patients with HIV-1. The WHO and EASL also incorporated DBS into their guidelines in 2016, simplifying sample collection and transport and increasing access to diagnostic testing.11,12
Case in point: Georgia
In 2015, the Republic of Georgia, a country with an estimated 5.4 percent of the adult population (approximately 150,000 persons) chronically infected with HCV, declared that it would eliminate HCV (defining elimination as a 90 percent reduction in HCV prevalence) from within its borders by 2020.14 Following the first year of the program (April 2015–April 2016), a total of 27,595 persons initiated treatment for HCV infection, among whom 19,778 (71.7 percent) completed treatment. Among 6,366 persons tested for sustained virologic response, 5,356 (84.1 percent) had achieved this milestone.15 Despite the availability of effective antiviral medications, however, the number of people enrolling in therapy declined toward the end of 2016.16
To reach the 2020 elimination goal of 90 percent reduction in HCV prevalence, efforts need to begin with increased measures to diagnose infected persons and link them to care and treatment. To explore diagnostic modalities, the Georgian National Center for Disease Control (NCDC), U.S. Centers for Disease Control and Prevention (CDC), and Abbott conducted studies to evaluate the concordance between HCV RNA and HCV antigen tests between 98.5 percent and 100 percent for confirmation of active infection, treatment monitoring, and determination of cure. The use of HCV antigen tests reduced diagnostic costs by 50 percent and simplified the testing with a rapid low-complexity method.17
HBV diagnostics and treatments
While curative therapies are not available for the 257 million people worldwide who are chronically infected with HBV, treatments are available to suppress the virus and manage infection, significantly reducing morbidity and mortality. People who are infected with HBV after age five have between a six percent and 10 percent risk of developing chronic hepatitis B.18 In the 1980s, an effective vaccine was introduced to protect against new infection.
Accurate diagnosis of HBV infection can be complex and involve multiple markers. Initial screening involves testing for the HBV surface protein (HBsAg), antibody to the HBV surface protein (anti-HBsAg), and antibody to HBV core protein (anti-HBc). A HBsAg positive, anti-HBsAg negative result with anti-HBc positive indicates an active HBV infection. If the HBsAg positive result persists for greater than six months, it is considered a chronic HBV infection. If HBsAg is negative while anti-HBsAg and anti-HBc is positive, the patient has recovered from a past infection with immunity.19
Because HBV is highly infectious, it is very important for people with the infection to know their status in order to take steps to prevent transmission to other people. This is particularly important for pregnant mothers, as vertical or perinatal transmission is a major driver of new infections, particularly in resource-limited settings, and this route of transmission results in more than 90 percent of chronic infections. Fortunately, there are effective interventions that can drastically reduce the rate of mother-to-child transmission. These interventions include diagnosis of the pregnant mother early enough to provide antiviral therapy to suppress the virus prior to birth and then providing the infant with a birth dose of HBV vaccine as well as a dose of HBV immunoglobulin (HBIG).20
HBV is a dynamic disease, and once diagnosed all infected people should be monitored regularly. Additional markers, including HBV “e” protein (HBeAg) and HBV DNA, indicate levels of viral replication in the liver. In addition, aminotransferase enzyme “ALT,” which is indicative of the level of liver inflammation and damage, should be tested regularly to assess whether treatment is necessary and, once therapy is initiated, should be used to monitor response to therapy. While there is no clinical cure for chronic HBV infection, a functional cure can be achieved, and this is defined as the suppression or elimination of HBV DNA with HBsAg loss and appearance of antibodies to HBsAg. Currently very few people (one percent to three percent per year) meet this criterion for functional cure, and EASL recommends stopping treatment in those people who achieve HBsAg loss even in the absence of anti-HBsAg.21
Improvements in HBsAg assay sensitivity approaching the performance of nucleic acid testing (NAT) may impact the number of people who have treatment-induced undetectable HBsAg and are essential to further reduce the detection window for acute HBV infection in regions where NAT is not widely available. Additionally, the sensitive detection of HBsAg mutants that continue to evolve due to vaccine escape, therapies, natural immune selection, and an error-prone reverse transcriptase is a necessity. In the absence of HBsAg loss, with appropriate antiviral treatment, most people can achieve undetectable HBV DNA status, and approximately 21 percent achieve HBeAg seroconversion. That is, HBeAg-positive patients achieve HBeAg loss with the appearance of antibodies to HBeAg after 12 months of treatment with a potent nucleoside analogue therapy, which indicates that the immune system is fighting the infection and reducing viral replication.22
There is great excitement in the field as researchers push for novel therapeutic approaches that might increase the number of patients who achieve a functional cure and may even result in clinical cure for HBV infection. These approaches target every stage of the virus life cycle and include direct antivirals such as silencing RNA (siRNA), entry inhibitors, capsid inhibitors, HBsAg inhibitors and cccDNA inhibitors or indirect antivirals such as therapeutic vaccines, “toll like receptor” (TLR) agonists, and cyclofinin inhibitors. Next-generation therapies for HBV will most likely involve a combination of these drugs. Within the diagnostics industry, parallel research is ongoing into novel tests such as HBV pre-genomic RNA, ultrasensitive HBsAg, and HBV core protein. When used in conjunction with tests already available, those provide clinicians and drug developers with insights into the effect new therapeutic approaches have on the virus, assisting in the development of novel treatment regimens and informing how these tests might be used to optimize patient outcomes.
A key lesson from the HIV epidemic is that treatment of this disease alone is not enough to win the battle. Instead, comprehensive approaches to prevention and treatment have led to the extensive progress made in the last decade. Similarly, with HBV and HCV, new approaches to diagnostics, surveillance, and treatment must be undertaken to eliminate viral hepatitis by 2030.
REFERENCES
- HIV/AIDS fact sheet. World Health Organization (WHO). http://www.who.int/mediacentre/factsheets/fs360/en/
- HCV fact sheet. WHO. http://www.who.int/mediacentre/factsheets/fs164/en/
- HBV fact sheet. WHO. http://www.who.int/mediacentre/factsheets/fs204/en/
- 90-90-90: An ambitious treatment target to help end the AIDS epidemic. UNAIDS. http://www.unaids.org/en/resources/documents/2017/90-90-90
- Combating hepatitis B and C to reach elimination by 2030: Advocacy Brief. WHO. http://www.who.int/hepatitis/publications/hep-elimination-by-2030-brief/en/.
- Mizokami M, Yokosuka O, Takehara T, et al. Ledipasvir and sofosbuvir fixed-dose combination with and without ribavirin for 12 weeks in treatment-naive and previously treated Japanese patients with genotype 1 hepatitis C: An open-label, randomized, phase 3 trial. Lancet Infectious Disease 2015;15(6):645-53. doi: 10.1016/S1473-3099(15)70099-X.
- Younossi ZM, Park H, Gordon SC, et al. Real-world outcomes of ledipasvir/sofosbuvir in treatment-naive patients with hepatitis C. American Journal Managed Care. 2016;22(6 Spec No.):SP205-211.
- Grebely J, Raffa J, Lai C, et al. Factors associated with spontaneous clearance of hepatitis C virus among illicit drug users. Canadian Journal Gastroenterology. 2007;21(7): 447–451.
- Icardi G, Ansaldi F, Bruzzone BM, et al. Novel approach to reduce the hepatitis C virus (HCV) window period: clinical evaluation of a new enzyme-linked immunosorbent assay for HCV core antigen. Journal Clinical Microbiology. 2001;39(9):3110–3114.
- Hans R, Marwaha N. Nucleic acid testing—benefits and constraints. Asian Journal Transfusion Science. 2014;8(1): 2-3.
- WHO guidelines on hepatitis B and C testing. Geneva: World Health Organization; 2017. License: CC BY-NC-SA 3.0 IGO.
- EASL recommendations on treatment of hepatitis C. 2017. Journal of Hepatology. 66:153-194. http://dx.doi.org/10.1016/j.jhep.2016.09.001.
- Mohamed Z, Mbwambo J, Shimakawa Y, et al. 2017. Clinical utility of HCV core antigen detection and quantification using serum samples and dried blood spots in people who inject drugs in Dar-es-Salaam, Tanzania. Journal International AIDS Society.2017;20(1):21856. doi: 10.7448/IAS.20.1.21856.
- Gvinjilia L, Nasrullah M, Sergeenko D, et al. National progress toward hepatitis C elimination—Georgia, 2015-2016. Morbidity and Mortality Weekly Report. 65(41):1132-1135. doi: 10.15585/mmwr.mm6541a2.
- Nasrullah M, Sergeenko D, Gvinjilia L, et al. The role of screening and treatment in national progress toward hepatitis C elimination—Georgia, 2015-2016. Morbidity and Mortality Weekly Report. 2017;66(29):773-776. doi: 10.15585/mmwr.mm6629a2.
- Nasrullah M, Sergeenko D, Gamkrelidze A, Averhoff F. HCV elimination—lessons learned from a small Eurasian country, Georgia. Nature Reviews: Gastroenterology & Hepatology.2017;14(8):447-448.
- Drobeniuc J. International Liver Congress 2017 Amsterdam. The vital role of laboratory diagnostic services. Data presented at special session on Republic of Georgia HCV elimination.
- Hepatitis B FAQs for the public. U.S. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/hepatitis/hbv/bfaq.htm
- Adapted from: A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: Recommendations of the advisory committee on immunization practices. Part I: Immunization of Infants, Children, and Adolescents. Morbidity and Mortality Weekly Report. 2005;54:No. RR-16.
- Hepatitis B information: Perinatal transmission. U.S. CDC. https://www.cdc.gov/hepatitis/hbv/perinatalxmtn.htm
- Lampertico P, Agarwal K, Berg T, et al. Clinical practice guidelines on the management of hepatitis B virus infection. Journal of Hepatology. 2017;67(2): 370-398.
- Papatheodoridis G, Vlachogiannakos I, Cholongitas E, et al. Discontinuation of oral antivirals in chronic hepatitis B: a systematic review. Journal of Hepatology. 2016;63(5):1481-1492. doi: 10.1002/hep.28438.
Gavin A. Cloherty, PhD, serves as Director of Infectious Disease Research for Abbott’s diagnostics business.