CONTINUING EDUCATION
To earn CEUs, visit www.mlo-online.com under the CE Tests tab.LEARNING OBJECTIVES
1. Discuss heart failure (HF) healthcare statistics in the United States.
2. Explain the diagnostic evaluation of natriuretic peptides and the uses of them in acute and non-acute settings.
3. Discuss drug management of patients with HF.
4. Identify the cardiac marker studied and the outcome of the results in the sidebar article.
With an estimated 26 million people worldwide affected by heart failure (HF),1 the consequences of the syndrome present a growing challenge, not only to patients and physicians but to healthcare and insurance systems, as well as formal and informal caregivers.2 Hospital admissions for HF are the most common diagnosis-related group in the United States and are responsible for approximately five percent of all acute hospital admissions in Europe.3 Although hospitalization rates in the U.S. and Europe may have peaked in the first decade of the 21th century, long-term survival remains poor in patients with HF, and the rate of adoption of evidence-based therapies is still suboptimal.4 This complex syndrome can be compared to patients with malignant tumors, who have a similar mortality rate of 50 percent over three years.
Healthcare providers need to continually assess how to use resources in the most efficient way to manage the growing number of HF patients. Yearly costs attributable to HF in the U.S. are estimated at $32 billion, including the cost of healthcare services, medication, and lost productivity, and they are expected to triple by 2030.5 Approximately 80 percent to 90 percent of costs are associated with chronic cases.6 Not only are direct care costs high, but a study in Germany showed that indirect costs account for an additional 40 percent of overall HF-related expenditures.7 New and emerging techniques in imaging and diagnostics, as well as value-based care delivery, are providing physicians with powerful tools to diagnose and manage HF more efficiently.
Definition of HF
HF is a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood. The cardinal manifestations of HF are dyspnea and fatigue, which may limit exercise tolerance, and fluid retention, which may lead to pulmonary and/or splanchnic congestion and/or peripheral edema. Some patients have exercise intolerance but little evidence of fluid retention, whereas others complain primarily of edema, dyspnea, or fatigue. Because some patients present without signs or symptoms of volume overload, the term “heart failure” is preferred over “congestive heart failure.” There is no single diagnostic test for HF because it is largely a clinical diagnosis based on a careful history and physical examination. However, both the natriuretic peptides and imaging studies are extremely useful in the diagnosis of patients suspected of heart failure.8
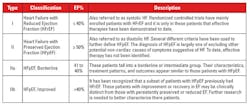
The clinical syndrome of HF may result from disorders of the pericardium, myocardium, endocardium, heart valves, or great vessels, or from certain metabolic abnormalities, but most patients with HF have symptoms due to impaired left ventricular (LV) myocardial function. Ejection fraction (EF) is considered important in classification of patients with HF because of differing patient demographics, comorbid conditions, prognosis, and response to therapies (Table 1).
Ejection fraction is the fraction of blood ejected from a ventricle of the heart with each heartbeat. The LV is the heart’s main pumping chamber that pumps oxygenated blood through the ascending (upward) aorta to the rest of the body, so EF is usually measured only in the left ventricle. An LV EF of 55 percent to 70 percent is considered normal. An LV EF of 50 percent or lower is considered reduced, and an EF of less than 40 percent is generally considered consistent with HF.8
Causes and classification of HF
The etiology of HF is diverse. There is no agreed single classification system for the causes of HF, with much overlap between potential categories (Table 2). Many patients will have several different pathologies that include both cardiovascular and non-cardiovascular causes at the origin of HF. Identification of these diverse pathologies should be part of the diagnostic workup, as they may offer specific therapeutic opportunities.9
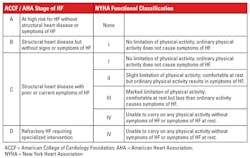
There are two major classifications of HF: the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) and the New York Heart Association (NYHA) classifications.10 Both the ACCF/AHA stages of HF and the NYHA functional classifications provide useful and complementary information about the presence and severity of HF (Table 3). The ACCF/AHA stages of HF emphasize the development and progression of disease and can be used to describe individuals and populations, whereas the NYHA classes focus on exercise capacity and the symptomatic status of the disease.8 Even though the ACCF/AHA classification is newer, the NYHA system appears to be used more frequently. Regardless of which system is used, progression in HF stages is associated with reduced five-year survival and increased plasma natriuretic peptide concentrations.11
Diagnostic evaluation of HF:natriuretic peptides
The diagnosis of HF can be difficult, especially in the early stages.12 Many of the signs and symptoms are non-specific and may be particularly difficult to identify and interpret in patients such as obese individuals, the elderly, or patients with chronic lung disease. It is therefore critical to the diagnosis that an underlying cardiac cause can be established or ruled out. Patients with HF often present with a wide differential diagnosis, making diagnosis by clinical presentation alone challenging. Some of the signs and symptoms, such as dyspnea, orthopnea, and paroxysmal nocturnal dyspnea, are due to congestion, while some are due to lack of adequate cardiac output, including fatigue, weakness, and exercise intolerance.
This heterogeneity of presentation often results in delays in definitive diagnosis and treatment, and such delays are linked with poor prognosis.13 Thus, together with HF’s risk for death and hospitalization, the growing incidence and prevalence make it a priority.
The natriuretic peptides (NPs) are markers of hemodynamic stress on the heart, denoting the neurohumoral activation of the myocardium. B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP) are the two brain NPs that are derived from the prohormone, proBNP. BNP and NT-proBNP are produced in a 1:1 ratio when the left ventricle is stretched due to hemodynamic pressure.
BNP and NT-proBNP are synthesized mainly in the ventricular myocardium in response to myocardial wall stress. BNP is a neurohormone that acts to relieve the symptoms associated with volume expansion and pressure overload by promoting natriuresis and diuresis, vasodilation, and the suppression of the renin angiotensin aldosterone system. BNP is termed brain natriuretic peptide because it was initially discovered in the porcine brain. Both BNP and NT-proBNP levels in the blood are used for screening and diagnosis of acute congestive heart failure (CHF) and may be useful to establish prognosis in HF, as both markers are typically higher in patients with worse outcomes. But the non-cleaved intact proBNP is also present in the circulation and represents a substantial part of the BNP and NT-proBNP immunoreactivity.14 The optimal application of NP testing is in conjunction with a good history, physical exam, and knowledge of the differential diagnosis of an elevated NP value. NP values are proportional to morbidity and mortality. (Figure 1)
NPs in dyspnea testing in non-acute settings
Non-specific symptoms do not help clinicians discriminate between HF and other clinical issues.15 Signs and symptoms of HF due to fluid retention may resolve quickly with diuretic therapy. Signs such as elevated jugular venous pressure and displacement of the apical impulse may be more specific, but they are harder to detect and have poor reproducibility. As noted above, signs and symptoms may be particularly difficult to identify and interpret in obese individuals, in the elderly, and in lung disease patients.15
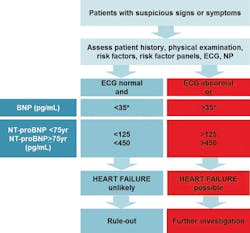
A detailed history should always be obtained. HF is unusual in an individual with no relevant medical history (e.g., a potential cause of cardiac damage), whereas certain features, particularly previous myocardial infarction, greatly increase the likelihood of HF in a patient with appropriate symptoms and signs. At each visit, signs and symptoms of HF need to be assessed, with particular attention to evidence of congestion. In non-acute settings, the types of patients who would most benefit from NP testing include patients with symptoms of dyspnea, patients with known coronary artery disease, patients with diabetes, patients with hypertension, and patients older than 60 years of age8,16-18 (Figure 2)
Testing in acute settings24
The workup of patients suspected of HF in acute settings is somewhat different from that which applies to those who present in non-acute settings. The majority of patients who present to the Emergency Department (ED) with HF are admitted to the hospital. This approach is largely due to the challenge of identifying ED patients at low risk for poor outcomes. Risk stratification of patients with acute HF is traditionally problematic, not only because of the patients’ underlying HF, but also because of their multiple comorbidities. Further, even for patients who exhibit no objective markers of high risk, the subsequent inability to ensure close follow-up, provide bedside HF education, and address the importance of adherence to therapeutic recommendations makes direct ED discharge problematic.
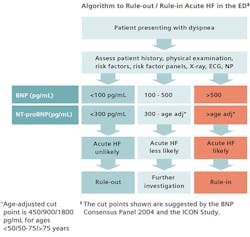
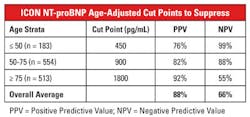
Because most patients hospitalized for acute HF present to the ED, emergency medicine physicians have become the gatekeepers for patients suspected of acute HF. ED patients with acute HF can be largely assigned to either of two groups based on presentation blood pressure: hypertensive patients (>140 mm Hg) and normotensive patients (<140 mm Hg). Hypotension (<90 mm Hg) and cardiogenic shock are rare and make up less than five percent of ED presentations.25,26 Therefore, patients arriving at the ED with dyspnea and/or chest pain or who are suspected of having heart failure should be tested with BNP or NT-proBNP and possibly imaging studies. (Figure 3)In 2006, Januzzi et al published a very important paper which evaluated the use of NT-proBNP in 1256 patients with dyspnea suspected of HF.28 This was a multi-center study to determine NT-proBNP cut-points for diagnosis or exclusion of acute HF and to evaluate the prognostic significance of elevated NT-proBNP in the setting of acute HF. The results of this study with regard to NT-proBNP are summarized in Table 4.
Using the single, age-independent rule-out cut-point of 300 ng/mL, the authors found that NT-proBNP had a negative predictive value (NPV) of 98 percent. In order to improve both sensitivity and specificity to rule-in HF, the authors found the age-related cut-points were better than any single value. This relationship between age and natriuretic peptide levels is likely consequent to age-related changes in LV compliance,29 as well as decreasing glomerular filtration rate (GFR).30 Although age stratification improved the ability of NT-proBNP to identify patients with high likelihood of acute HF, the authors found no need for age stratification to exclude the diagnosis of HF.
The optimal application of NP testing is in conjunction with a good history, physical exam, and knowledge of the differential diagnosis of an elevated NP value. The measurement of NPs has a direct impact on patient management.31,32 When used in conjunction with other clinical information, measurement of NPs in an acute setting improves the care of acutely dyspneic patients and reduces time to discharge as well as total cost of treatment. NP levels typically decrease rapidly in patients responding favorably to therapy.
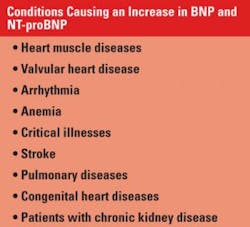
While the clinical utility of the NP has been well established, NP elevations can be observed in conditions other than HF and acute coronary syndrome (ACS) (Table 5), justifying the mandatory incorporation of all clinical data into the NP result interpretation. Importantly, these elevations of the natriuretic peptides should not be perceived as false positive results due to their associated strong prognostic values.33,34
Management of patients with HF
HF is sub-classified based on the left ventricular ejection fraction. HF with a reduced ejection fraction (HFrEF) is characterized by a left ventricular ejection fraction (LVEF) of less than 40 percent. Conversely, HF with preserved ejection fraction (HFpEF) is characterized by a normal LVEF and an impairment of cardiac relaxation with abnormal ventricular filling. Conventional therapies have been targeted to treat patients with HFrEF. These include angiotensin-converting enzyme inhibitors (ACEis) and, when ACEis are contraindicated, angiotensin receptor blockers (ARBs) and loop diuretics. These are considered first-line pharmacotherapy because they have repeatedly been shown to reduce death and hospitalizations significantly and improve exercise tolerance, functional capacity or status, LVEF, and quality of life.8
Even though the current drugs used to treat heart failure work reasonably well, there is still room for improvement by further reducing the mortality rate. For a period of 10 years, the FDA did not approve any new drugs for the chronic treatment of HF. In July 2015, the agency approved a new drug for the treatment of patients with HFrEF. This drug is currently marketed by Novartis under the brand name Entresto.34 Entresto is actually a combination of two drugs: valsartan, which is an angiotensin II receptor blocker, and sacubitril, which is a neprilysin inhibitor.35 This combination of drugs is also known as an angiotensin receptor blocker neprilysin inhibitor or ARNI.
The mechanism of action of Entresto is very interesting and has some profound effects on the natriuretic peptides. Valsartan blocks the angiotensin II receptor, causing vasodilation; reduces secretion of vasopressin; and reduces production and secretion of aldosterone, among other actions. The combined effect reduces blood pressure. Sacubitril is metabolized to a substance that inhibits neprilysin, which is responsible for the degradation of BNP, thereby causing a rise in the levels of BNP. Elevation of BNP levels increases the
beneficial effects of removing extracellular fluid via natriuresis, diuresis, and vasodilation, inhibiting production of renin and aldosterone and stimulating growth of vascular myocytes. Neither sacubitril nor its metabolites seem to have any effect on NT-proBNP levels.36
What is the net effect on natriuretic peptides in patients being treated with Entresto? Despite significant clinical improvement, BNP levels will tend to increase in patients being treated with Entresto. This increase in BNP levels may be confusing to physicians who may have become accustomed to levels decreasing as the patient shows clinical improvement. Since Entresto has no effect on the degradation of NT-proBNP, the levels of this NP will show the usual decrease, which follows clinical improvement in the patient.37,38
Both BNP and NT-proBNP are readily available in the modern clinical laboratory. Therefore, which NP should physicians use in routine clinical practice? In patients not being treated with Entresto, both BNP and NT-proBNP provide useful information to assist in the diagnosis of patients suspected of having HF. It should be noted that BNP and NT-proBNP have better diagnostic utility as rule-out tests. In patients receiving Entresto therapy, NT-proBNP will decrease, mimicking clinical improvement in the patient. BNP will tend to increase in response to sacubitril administration despite clinical improvement.8 Some recent publications demonstrate that the single measurement of BNP and/or NT-proBNP cannot provide a comprehensive biological and clinical picture for patients under Entresto.14,39 However, despite these differences, the physician will ultimately make the choice. The therapeutic use of Entresto for the treatment of patients with HFrEF was supported in a recent update to the HF guidelines.40 These guidelines strongly recommended treatment of patients with HFrEF with an ARNI in order to reduce morbidity and mortality in this group of patients.
The road ahead
As healthcare systems are in a transition from service-based to value-based models, concepts of prevention or early diagnosis become increasingly important; therefore the use of biomarkers (and advanced imaging) have gained significance. Participants in the expert panel agree that in the field of HF both have a central role in therapy guidance as in ACS.
To further establish new standards of HF care, new and innovative biomarkers guide differentiating diagnoses and therefore should be used as an early detection tool, as well as for monitoring and outpatient care. Biomarkers such as NT-proBNP can indicate diagnostic pathways, and a multi-biomarker panel could offer further diagnostic value.
REFERENCES
- Ambrosy AP, Fonarow GC, Butler J, et al. The global health and economic burden of hospitalizations for heart failure. J Amer Coll Cardiol. 2014;63(12):1123-1133.
- Clark AM, Reid ME, Morrison CE, Capewell S, Murdoch DL, McMurray JJ. The complex nature of informal care in home-based heart failure management. J Adv Nurs. 2008;61(4):373-383.
- Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure? Europace. 2011;13:ii13–ii17.
- Jhund PS, MacIntyre K, Simpson CR, et al. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: A population study of 5.1 million people. Circulation. 2009;119(4):515-523.
- Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: A policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3): 606-619.
- Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the united states a policy statement from the american heart association. Circulation. 2011;123(8):933-944.
- Neumann T, Biermann J, Erbel R, et al. Heart failure: the commonest reason for hospital admission in Germany. Dtsch Arztebl Int. 2009;106(16):269-275.
- Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. October 15, 2013; e240-e327.
- Lippi G Sanchis-Gomar F. Monitoring B-type natriuretic peptide in patients undergoing therapy with neprilysin inhibitors. An emerging challenge? Int J Cardiol. 2016;219:111-114.
- Hunt SA, Abraham WT, Chin MH, et al. 2009 focused update incorporated into the ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;119(14):e391-479.
- Ammar KA, Jacobsen SJ, Mahoney DW, et al. Prevalence and prognostic significance of heart failure stages: application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation. 2007;115(12):1563-1570.
- McMurray JJV, Adamopoulos S, Anker SD, et al., ESC Committee for Practice Guidelines (CPG). Bax JJ, Baumgartner H, Ceconi C, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Euro Heart J. 2012;33(14):1787-1847.
- Maisel AS, Peacock WF, McMullin N, et al. Timing of immunoreactive B-type natriuretic peptide levels and treatment delay in acute decompensated heart failure: an ADHERE (Acute Decompensated Heart Failure National Registry) analysis. J Am Coll Cardiol. 2008;52(7):534-540.
- Semenov AG,. Katrukha AG. Different susceptibility of B-type natriuretic peptide (BNP) and BNP precursor (proBNP) to cleavage by neprilysin: The N-terminal part does matter. Clin Chem. 2016;62(4):617-622.
- Ponikowski P. Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Euro Heart J. (2016) 37(27):2129-2200.
- Hildebrandt P. Natriuretic peptides: prediction of cardiovascular disease in the general population and high risk populations. Dis Markers. 2009;26(5-6):227-233.
- Hildebrandt P., Collinson, PO. Amino-terminal pro-B-type natriuretic peptide testing. Am J Cardiol. 2008;101(3A):25-28.
- Hildebrandt P, Collinson PO. Amino-terminal pro-B-type natriuretic peptide testing to assist the diagnostic evaluation of heart failure in symptomatic primary care patients. Am J Cardiol. 2008;101(suppl):21A-24A.
- Siemens Healthcare Diagnostics. ADVIA Centaur® BNP Instructions for Use. Tarrytown, NY, US: 2017.
- Siemens Healthcare Diagnostics. Dimension® HM NT-proBNP Instructions for Use. Tarrytown, NY, US: 2017.
- Remme WJ1, Swedberg K. The task force for the diagnosis and treatment of chronic heart failure of the European Society of Cardiology. Eur Heart J. 2005; 26(11):1115-1140.
- de Lemos JA, Hildebrandt P. Amino-terminal pro-B-typer natriuretic peptides: testing in general populations. Am J Cardiol. 2008;101(suppl):16A-20A
- Wang TJ, Larson MG, Levy D, et al. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med. 2004;350(7):655-63.
- Weintraub NL, Collins SP, Pang PS, et al. Acute heart failure syndromes: emergency department presentation, treatment, and disposition: current approaches and future aims a scientific statement from the American Heart Association. Circulation. 2010;122(19):1975-1996.
- Gheorghiade M, Abraham WT, Albert NM, et al. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA. 2006;296(18):2217–2226.
- Peacock WF, Fonarow GC, Ander DS, et al. Society of Chest Pain Centers Recommendations for the evaluation and management of the observation stay acute heart failure patient: a report from the Society of Chest Pain Centers Acute Heart Failure Committee. Crit Pathw Cardiol. 2008;7(2):83–86.
- Nieminen MS, Bohm M, Cowie MR, et al. Executive summary of the guidelines on the diagnosis and treatment of acute heart failiure: The Task Force on Acute Heart Failure of the European Society of Cardiology. Eur Heart J. 2005;26(4):384-416.
- Januzzi J, van Kimmenade R, Lainchbury J, et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients. The International Collaborative of NT-proBNP Study. Euro Heart J. 2006;27(3):330-337.
- Arbab-Zadeh A, Dijk E, Prasad A, et al. Effect of aging and physical activity on left ventricular compliance. Circulation. 2004;110(13):1799-1805.
- McCullough PA, Duc P, Omland T., et al. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis. 2003;41(3):571-579.
- Bettencourt P, Januzzi JL Jr. Amino-terminal pro–B-type natriuretic peptide testing for inpatient monitoring and treatment guidance of acute destabilized heart failure. Am J Cardiol. 2008;101(suppl):67A-71A.
- Jourdain P, Jondeau G, Funck FA, et al. Plasma brain natriuretic peptide-guided therapy to improve outcome in heart failure: the STARS-BNP Multicenter Study. J Am Coll Cardiol. 2007;49(16):1733-1739.
- Baggish AL, van Kimmenade RR, Januzzi JL Jr. The differential diagnosis of an elevated amino-terminal pro-B-type natriuretic peptide level. Am J Cardiol. 2008;101[suppl]:43A-48A.
- van Kimmenade RRJ, Pinto YM, Bayes-Genis AJ, Lainchbury JG, Richards AM, Januzzi JL. Usefulness of intermediate aminoterminal pro-brain natriuretic peptide concentrations for diagnosis and prognosis of acute heart failure. Am J Cardiol. 2006;98(3):386-390.
- McMurray JJV, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. New Engl J Med. 2014;371(11):993-1004.
- Mechanism of action: entresto. https://www. Entrestohcp.com/mechanism-of-action.
- Novartis’ new heart failure medicine LCZ696, now called Entresto(TM), approved by FDA to reduce risk of cardiovascular death and heart failure hospitalization. https://www.novartis.com/news/media-releases/novartis-new-heartfailure-medicine-lcz696-now-called- Entrestotm-approved-fda
- McMurray, J. Angiotensin receptor-neprilysin inhibition (ARNI): The new frontier? https://image.slidesharecdn.com/arnis-the-new-frontier-160211122620/95/angiotensin-receptorneprilysin-inhibitionarnithe-new-fronteir-13-638.jpg?cb=1455193899.
- Lippi G, Sanchis-Gomar F. Monitoring B-type natriuretic peptide in patients undergoing therapy with neprilysin inhibitors. An emerging challenge? Int J Cardiol. 2016;219:11-114
- Yancy, CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2016;68(13):1476-1488
Jim Aguanno, PhD, serves as Senior Clinical Consultant for Siemens Healthineers.
Laurent Samson, PhD, serves as Associate Director, Global Commercial Marketing, for Siemens Healthineers.