Achieving value: Community outreach and other strategies for labs
Recent market estimates indicate that, today, more than 70 percent of healthcare is delivered outside of the four walls of a hospital.1 With this trend, managing outpatient care and attracting business from community providers are more important than ever as healthcare organizations strive to maintain a healthy balance sheet. Laboratories must work to change the way they often are perceived by the administrators of their larger institution—to show that they should be viewed not as a cost center but as a value center. Effective use of software both inside the institution and to reach out to the community is a key to success.
With the right tools and planning, laboratories can position themselves as a strategic growth lever in a healthcare organization. Going beyond mere cost cutting, laboratories can optimize utilization to create efficiencies and develop their services to be used by external care facilities—thus helping to drive additional revenue across the entire healthcare organization. Achieving this goal requires three strategies: streamlining workflows, improving productivity, and securing outreach business from care providers in the community.
Streamlining workflows
When test volume fluctuates, a laboratory often has more resources than it would require if it had the same volume more evenly spread. Methodologies such as Lean and Six Sigma can help laboratories streamline their workflow and optimize their resources, helping them achieve a higher quality of service at a lower cost. A recent report2 highlighted one organization’s success using such principles. After a review of current procedures, Jackson Health System found multiple instances of inefficiencies and expensive procedures in its laboratory. Using Lean principles, lab leaders planned a full redesign of their work space that improved turnaround times, maximized flow, eliminated waste, and reduced inventory/supplies and costs.
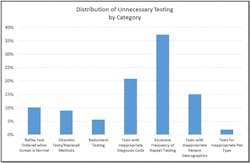
Another way to eliminate unnecessary and costly procedures is by leveraging a strong laboratory information system (LIS) to manage the utilization of laboratory tests. There is almost always some unnecessary testing going on, and knowledge is power when it comes to minimizing that (Figure 1).3
Laboratory tests play a significant role in the majority of diagnosis and treatment decisions. The right tests can lead to fewer errors, faster diagnoses, and better patient care. The LIS can reduce costs by guiding the care provider to more targeted tests and eliminating erroneous testing and retesting as a result of ordering the wrong tests. Where over-testing can be costly to a healthcare organization, under-testing can be even more expensive, with some estimates putting it at close to 38 percent of total healthcare costs.4 On average, 43 percent of diabetes patients won’t respond to initial treatment.5 The right laboratory tests can help identify more effective treatments for these patients, reducing avoidable readmissions and the total cost of patient care. Patients will benefit from faster treatment times and a quicker road to more effective disease management.
Improving productivity
The University of Miami Health System recently improved productivity by standardizing workflows for physicians, patients, and laboratory staff throughout the entire system.6 These prescribed workflows used consistent processes and instrumentation and enabled them to optimize their staff, specifically, by allowing staff to be easily transferred from site to site with very little impact.
Other improvements in productivity can be made by leveraging LISs. A fully automated lab can increase volume with minimum impact to the cost per test 7 by reducing human error, while creating a more organized and connected system. These systems can automate collection and specimen labelling. Labs can better track specimens, even when originating from multiple facilities, through integrated specimen management functionality. LISs can also help match patients across systems to past records and reduce staff burden by providing lab results electronically to the ordering provider.
Securing outpatient work
According to a recent survey, initiatives directed towards patient care will ultimately be a more effective value differentiator.8 In order to garner greater interest, labs can link their services to patient outcomes by providing more consultative services. Services such as integrating clinical recommendations into laboratory reports, providing post-test interpretation consultations for complex tests, and collaborating on treatment plans help labs become more attractive due to their role in helping the care provider achieve a better patient outcome.
A robust, “best of breed” LIS can also provide the laboratory with more advanced capabilities and more meaningful data to aid in the management of patient outcomes across a diagnostic community. The right technology not only provides connectivity to the community providers for easier sharing of the clinical report, but also can provide the results in a way that a patient can understand them—a helpful asset to the care provider given the more competitive environment resulting from patient-driven care decisions. The LIS can also provide insightful analytics to further the collective goal of leveraging data to improve care for populations based on their disease-specific needs.
Laboratories can leverage these strategies to help the healthcare organization be more successful financially, while at the same time, catering to the diagnostic communities as a whole. That is a recipe for better patient outcomes across the care continuum, whether that care resides inside the hospital or out.
References
- Brown B, Burton D. The top trends that matter in 2014 [webinar]. March 19, 2014. http://www.healthcatalyst.com/webinar/the-top-trends-that-matter-in-2014. Accessed October 24, 2015.
- Michel RL, Christensen S. 2008 trends in clinical pathology laboratory management: ten trends that highlight rapid changes in healthcare & laboratory medicine. Dark Daily. http://www.darkdaily.com/wp-content/uploads/clinical-pathology-laboratory-trends-20081.pdf. Accessed October 24, 2015.
- Zhi M, Ding E, Theisen-Toupal J, et al. The landscape of inappropriate laboratory testing: a 15-year meta-analysis. PLOS One. 2013. doi: 10.1371/journal.pone.0078962.
- White L. The lab’s role in value-based pricing. Executive Insight. 2012 http://healthcare-executive-insight.advanceweb.com/Features/Articles/The-Labs-Role-in-Value-based-Pricing.aspx.
- Personalized Medicine Coalition. The case for personalized medicine. 2014 http://www.personalizedmedicinecoalition.org/Userfiles/PMC-Corporate/file/pmc_the_case_for_personalized_medicine.pdf. Accessed October 24, 2015.
- O’Toole M, Giuma J. Quality in the continuum of care. Executive Insight. 2015.
- Marwood research commissioned by Sunquest Information Systems, Inc. 2014.
- Xu J. Laboratory data in ACO environments. Clinical Lab Products. June 17, 2015. http://www.clpmag.com/2015/06/laboratory-data-aco-environments/. Accessed October 24, 2015.