What to do with expanded molecular testing capacity in a post-pandemic world
If ever there were a stress test designed just to assess a clinical lab’s agility, flexibility and performance, the COVID-19 pandemic would meet the specifications perfectly. Onboarding new diagnostic platforms and tests with little notice, managing unpredictable and rapidly escalating test volumes, meeting demands for quick turnaround time, and coping with fluctuating supply chains are just a few fundamental challenges imposed by SARS-CoV-2 testing. Forced to operate as reference labs for COVID-19 testing, many hospital-based labs spent most of 2020 ramping up their molecular testing capacity to meet demand. As the pandemic enters a new phase and COVID-19 testing needs decline dramatically, those same labs now face a new challenge: deciding what to do with the expanded testing capacity. Do they get rid of some platforms or repurpose them? And what criteria should they use to make these decisions?
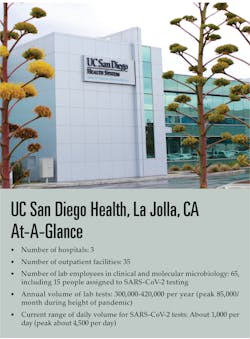
From zero to 4,500 tests a day
Our molecular diagnostics lab, part of UC San Diego Health’s full-service microbiology lab, underwent a significant structural change during the COVID-19 pandemic. As one of the earliest labs in the U.S. to start SARS-CoV-2 testing, we had an initial volume of 20 samples a day, which escalated rapidly to meet the demands not only of our own hospital and all first responders in San Diego, but also as a reference lab for other hospitals in San Diego and, importantly, all testing for transplant patients. Very quickly, we evolved a dual strategy: (a) to diversify our testing platforms and (b) to separate SARS-CoV-2 testing from other molecular lab operations by setting up a new lab. This strategy helped us manage a peak volume of 4,500 to 6,000 SARS-CoV-2 tests per day.
We implemented SARS-CoV-2 testing using real-time PCR on seven platforms from six different manufacturers, five of which were new acquisitions during the pandemic. This meant bringing one new SARS-CoV-2 test online a week, every week, until COVID-19 testing on all platforms went live. This planned diversification of platforms and manufacturers was driven in part by the somewhat limited availability of instruments and reagents, and, in part, by our own preference not to become overly dependent on one vendor during a time of unpredictable supply chains. In parallel with acquiring multiple platforms, we set up a separate facility dedicated to SARS-CoV-2 testing that is physically and operationally distinct from our molecular lab. We were fortunate to have an unused, newly constructed lab in a separate wing of our building — ready to start operation once power was connected and internet access was online.
Right from the start, we chose real-time PCR testing rather than antigen assays, even though both types of assays are available with emergency use authorization (EUA) from the U.S Food and Drug Administration (FDA). A comparative study in our lab showed that antigen-based assays may be insufficient to diagnose SARS-CoV-2 infection when lower levels of the virus are shed.1
Pooled testing for asymptomatic individuals was also integral to our testing strategy. (Specimens from symptomatic individuals were tested individually.) About a third to half of testing was done on pooled specimens. Separately, a point-of-care PCR test with a 15-minute turnaround time was also implemented. All told, our lab had completed close to 1 million SARS-CoV-2 tests by the end of June 2021.
Leveraging expanded lab capacity
With increased vaccination and slowing infection rates, the pandemic entered a new phase and the need for SARS-CoV-2 testing decreased. Like many labs that have built up capacity during the pandemic, our lab now looks toward leveraging our expanded capacity to enhance our services. We kept three goals in mind as we reviewed the platforms we have on hand to make decisions on how best to deploy them in the post-pandemic environment.
First and foremost is improving patient care and, thus, physician and patient satisfaction. Faster turnaround time is key to meeting this goal. Secondly, we saw the opportunity to maximize productivity through automation, and that means assessing each platform on its ability to reduce hands-on labor — for example, through pre-analytics automation capabilities. A third consideration is the menu.
Operationally, a broad menu enables us to streamline workflow and achieve greater efficiency. A broad menu also allows us to offer more choices of tests to our clinicians and, importantly, to reduce the number of tests we send out to other labs. Reducing send-outs decreases turnaround time and gets results in clinicians’ hands sooner. It also helps increase revenue and reduce costs. Along those lines, having a utility channel on our instrument platform gives us the ability to run lab developed tests (LDTs) more efficiently (i.e., on a fully automated, high-throughput system) and even more flexibility to support our clinicians.
These goals readily translate into criteria for weighing the relative strengths and weaknesses of each platform: menu, level of automation, and cost. A broad menu enables us to meet diverse testing needs on the same platform, streamlining the workflow and increasing lab efficiency and productivity. A higher level of automation (including pre-analytics) and higher throughput are key to improving workflow and freeing up highly trained, specialized molecular staff. As always, cost is a consideration, with financial performance being a key metric of a lab’s success.
During the pandemic, our prior experience with a fully automated, real-time PCR system was one reason behind our decision to bring a second, even higher-throughput system online. Post-pandemic, we dedicated one of the two systems to an expanded sexual health menu, including TV/MG (Trichomonas vaginalis and Mycoplasma genitalium), previously a send-out, and infectious disease testing (e.g., HIV-1/HIV-2 qualitative). The same system also handles transplant viral load testing. EBV (Epstein-Barr virus) and BKV (BK polyomavirus), previously only available as LDTs from our lab or as send-outs, will be run using FDA-cleared tests on our automated system, improving turnaround time. A second automated system is now dedicated to SARS-CoV-2 and influenza A/B testing, as well as a respiratory panel, in readiness for the upcoming respiratory season. A third older, lower-throughput and partially automated model of the same platform will be used as a backup.
The fourth platform, a real-time PCR system, with liquid handler added during the pandemic to meet testing demand, will be dedicated to research use in our human genetics lab and as part of our microbiome initiative. A fifth automated, real-time PCR system served us well for SARS-CoV-2 testing but will no longer be needed, primarily due to its limited menu, and will be set aside as a reserve system for future use. A sixth platform remains in use for SARS-CoV-2 testing, until all reagents are depleted. We discontinued the seventh platform when testing demand began to drop.
Conclusion
As we emerge from the pandemic, our added capacity opens the door to improved patient care, greater physician satisfaction, and more revenue opportunity as we leverage our fully automated systems to offer more tests at faster turnaround time and more streamlined lab operations. Looking ahead, pandemic preparedness will always be within our line of sight. Our experience and our expanded capacity are foundations for an effective response.
References
- Kuo P, Realegeno S, Pride DT. Comparison of two nucleic acid amplification tests (NAATs) and two antigen tests for detection of SARS-CoV-2 from upper respiratory specimens. J Clin Virol Plus. 2021 Jun; 1(1): 100011. doi.org/10.1016/j.jcvp.2021.100011.
About the Author

David T. Pride, MD, PhD
serves as Director of the Molecular Microbiology laboratory and the Associate Director of the Clinical Microbiology laboratory at UC San Diego Health, La Jolla, CA. Pride is board certified in Internal Medicine and received subspecialty training in Infectious Diseases at Stanford University.