People often confuse the terms variant, mutant and strain. A mutation is a single nucleotide change, which is introduced in the viral genome that leads to an amino acid change, while a variant is the viral genome that contains a particular set of mutations, and a strain is a variant that shows a differing phenotype, such as being more pathogenic or transmissible.1
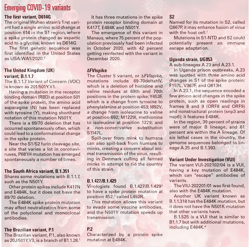
For example, the UK variant, known as B1.1.7, has 23 mutations with 17 amino acid changes. Thus, it is considered a strain, as it has evidence of being more infectious. An amino acid change, a deletion or an insertion into the spike protein, can result in a mutation. Mutations take place throughout the viral genome, but it’s not an equal occurrence, as there are “hotspots,” such as the spike protein.
The Centers for Disease Control and Prevention (CDC) has been receiving samples from various state departments and agencies for sequencing since Nov. 2020. They provide further characterization, sequencing and evaluation. At the end of January 2021, the National SARS-CoV-2 Strain Surveillance (NS3) system was ramped up to 750 samples a week from across the country, as the CDC contracts with large commercial diagnostic labs to sequence 6,000 samples per week, with the capacity to increase if need be. 1
Next-generation sequencing (NGS) and bioinformatics have been integrated into the public health system since 2014. Health departments apply for the resources during response to COVID-19, making genomic data available to public databases. In Dec. 2020, $15 million of COVID supplemental funds were released through the Epidemiology and Laboratory Capacity Program.
The CDC leads a national consortium of laboratories sequencing SARS-CoV-2 (SPHERES), which consists of more than 160 institutions, including academic centers, industry, non-governmental organizations, and public health agencies. This networking allows genomic data to be available through public databases for use by public health professionals and researchers. The FDA uses the health sequencing data to monitor mutations.
Sequencing and lab work
According to the FDA website, “the presence of mutations in the SARS-CoV-2 virus in a patient sample can potentially impact test performance. The impact of mutations on a test’s performance is influenced by several factors, including the sequence of the variant, the design of the test, and the prevalence of the variant in the population.”
With molecular tests, false negatives may occur if a mutation is in the part of the virus’ genome that is being detected by a test. Since molecular tests use multiple genetic targets, final results are not as likely to be impacted by genetic variants. When viral genome changes viral proteins, it can impact an antigen or serology test.
Treat the whole patient. If there is a negative result, but clinical observations show additional signs, the patient has a worrisome history, or epidemiological information makes you think otherwise, consider retesting with a different test, perhaps targeting different genetics, if COVID-19 is still suspected.
Laboratories around the globe struggle to keep up with the number of emerging variants. “In terms of the variants, we have been following guidelines from different governments and institutions, using resources like the FDA, CDC and World Health Organization, for variants of concerns, and we target those regions,” said Helen Roberts, PhD, President of Seegene Technologies, one of the many companies targeting variants for testing.
“Viruses often have mutations based on how prevalent a virus becomes. The more there is, the more likely there will be mutations, so mutations are not a surprise to the scientific community. It’s more about discovering where the mutations are and how they affect, as they usually adapt to give an advantage to the virus, a selection. It’s not surprising how fast the virus spreads. We have used an AI-based system to develop, and that’s our key ability: to quickly adapt to make assays,” explained Roberts.
There’s a vast amount to learn about variants, from finding how far they have spread, to knowing the similarities and differences between strains, which helps to recommend the best therapies, tests and vaccines.
“If a nucleotide is missing, a sequencing is different from one to the next.” Roberts shared how the differences impact an assay that can detect a deletion, as assays are designed to detect a specific protein sequence. If that sequence should change, “that change has a huge effect of how it hybridizes to find its target. We look for changes and deletions.”
Through genomic sequencing, genes are decoded, a key to making new discoveries. The sections, or genes, are encoded to build the virus, and this is how the changes to variants can be monitored over time, knowing their characteristics.
Synthetic genomes can be used to generate viruses to test vaccines. “Synthetic genomes are a much more reliable and scalable source of viruses than clinical samples, since clinical samples, when propagated extensively, often result in a mixture of virus population with multiple genomic changes,” explained Charlie Schmidt, Codex DNA Senior Director of Marketing. Synthetic genomes have also served as diagnostic controls in RT-PCR and NGS based assays.
Manoj Gandhi, MD, PhD, Senior Medical Director for Genetic Testing Solutions at Thermo Fisher Scientific suggested as the emphasis for SARS-CoV-2 strain identification increases, lab professionals will see an increased demand for surveillance testing.
“Conventional surveillance testing is performed by sequencing the viral genome. In some ways, sequencing can be considered as the ‘classic’ surveillance methodology. Since next generation sequencing (NGS) can provide the sequence of the entire viral genome, one can exactly know what the full sequence of the virus is. NGS is mostly useful if one would like to sequence the entire genome to discover ‘new’ or ‘emerging’ variants. In addition to NGS, one can also perform targeted sequencing of specific regions within the viral genome, such as the S-gene for example, using capillary electrophoresis, also commonly known as Sanger sequencing. Sanger sequencing can help rapidly verify and confirm the presence of specific mutations in the sample,” said Gandhi.
James Gilmore, CCO of SeqOnce Biosciences, said, “RT-qPCR testing for Variants of Concern is faster and less expensive than sequencing. Additionally, more labs have access to qPCR instruments, compared to sequencers, so using qPCR makes sense for surveillance.”
An assay is faster for labs to adopt than genomes. “It’s just a workflow,” Roberts explained. “The sample prep to read up is a longer workflow, and sequencing takes a few hours, so it’s a longer workflow than the assays,” which would be around two hours.
Government and private databases track variant impact on COVID-19 severity, as well as the effectiveness of vaccines and therapeutics. Researchers can track the variants’ ability to spread, cause milder or more severe symptoms, and evade detection through some diagnostic tests. Many popular nucleic acid amplification tests use reverse transcription polymerase chain reaction (RT-PCR), where there are multiple detection targets. Thus, if a mutation impacts one of the targets, the other RT-PCR targets will still work, but in tests relying on only one target, mutations may not be detected.
Challenges
“From a laboratory perspective, the mutations in these variants may impact the way some of the diagnostic tests are able to detect the presence of the virus. For example, the 69-70 deletion in the S-gene in the B.1.1.7 variant can result in a S-gene target failure (SGTF), also called as a S-gene drop out, in the TaqPath COVID-19 Combo Kit. However, due to the built-in redundancy of the assay with two other targets available for result calling, the overall sensitivity of the test should not be impacted. Moreover, the S-gene drop out may be used as surveillance tool as an indicator for the presence of the B.1.1.7 variant of concern,” said Gandhi.
“In light of the mutations that are occurring in different part of the viral genome, laboratory professionals need to make sure that these mutations are not impacting the PCR tests that have been deployed in their laboratory for SARS-CoV-2 detection. Laboratory professionals also need to evaluate tests as to which and how many targets does a specific test use for result calling. Multi target assays that target more than one region of the viral genome are generally preferable to single target assays, since it offers built-in redundancy in case one of the targets is impacted by a mutation.”
When testing for B.1.427/B.1.429, he added, “due to the presence of the L452R mutation, it may be associated with poor response to antibody-based therapies.”
Studies have shown spike-bearing viruses do not infect cells when soluble ACE2 is present, as it acts like a viral decoy, or with Camostate (Calu-3 cells), a TMPRSS2 inhibitor.1 A 13/14 sera from infected patients also produced potent neutralization of spike-driven entry into the host cell.
For molecular tests, the FDA noted the following molecular tests may be impacted by mutations:
- Accula SARS-CoV-2 test, Mesa Biotech, for a variant at position 28881 (GGG to AAC)
- Linea COVDI-19 Assay Kit, Applied DNA Sciences, impacted by B.1.1.7 mutations
- TaqPath COVID-19 Combo Kit, Thermo Fisher Scientific, reduced sensitivity to S-gene target
- Xpert Xpress SARS-CoV-2, Xpert Xpress SARS-CoV-2 DoD, and Xpert Omni SARS-CoV-2, Cepheid, which has sensitivity detecting the N2 target3
Most developing vaccines are either mRNA, adenoviral or recombinant protein, and all currently approved vaccines targets the spike protein; thus, a RBD-based assay has to be used when determining a vaccine antibody response when the nucleoprotein is not a part of it.
Studies of the mRNA-1273 vaccine against various variants4 revealed a decrease in titers of neutralizing antibodies against B.1.351,5 but it had no real effect on B.1.1.7. Levels of neutralization against D614 were similar to strains EU1, 20A.EU2, N439K-D614G and the cluster 5 variants.
The Janssen vaccine is based on older vaccine technology using a cold virus to deliver instructions to make the spike protein used by the COVID-19 virus, triggering an immune response and the development of antibodies. Similar technology was used to make the vaccine against Ebola. The Moderna and Pfizer vaccines differ, as they deliver mRNA instructions for the spike protein inside of a lipid ball that enters cells, creating the immune system.6
With so many developments on a fast learning curve, it’s tough for laboratories to keep up with the latest about variants and mutations. “There isn’t really a resource like the FDA EUA website, so it’s more challenging. Companies market themselves, because the FDA hasn’t consolidated and authorized for clinical use yet. It’s all for research use. The FDA is still recommending sequencing for variant typing, but not all laboratories have access to that,” said Roberts.
Gilmore said, “from a pandemic standpoint, we seem to be in a game of ’whack-a-mole’ for developing assays to detect the SARS-CoV-2 mutations. New mutations are being reported almost daily. This has made SeqOnce Biosciences re-think how to approach our assay development by making it more routine, ordering multiple probe/primer designs simultaneously (rather than sequentially), and streamlining the manufacturing process (e.g. conserving plasticware, maintaining consistent formulations and master mixes).” SeqOnce Biosciences has RT-qPCR assays for the CDC SARS-CoV-2 Variants of Concern (VOC), including: N501Y, E484K, and K417 wild type. They are also in the process of developing assays to detect variants E484Q, Q677H, and F888L.
“This is still very new,” explained Roberts. “Most labs are not testing yet. Now, there’s a few of us that have released tests, and it’s important for researchers to know there are several now available as a tool for them.”
Roberts stressed the important for surveillance and epidemiology to see if variants of concern are circulating in an area, as some are more resistant to vaccines. “So, be aware of what is circulating in the client pool, and be aware assays are available as a tool for them. PCR’s are easier than assays for labs to adopt if they are not already set up for sequencing.”
Advice for labs
“Labs should be aware that variants of concern may have multiple mutations of interest. As an example, there are reports of ‘double mutation,’ where a variant in India was positive for both L452R and E484Q,” said Gilmore.
“It’s very important for labs to understand the assays they’re using,” Roberts stressed, “as a few have been noted to have performances changed, so it’s important for labs to understand what assays they’re using and what part of the gene they are detecting. So, if they see a weird pattern, is this a variant issue, or something else?”
For tracking lineages, sequencing is good for identifying new mutations; whereas, PCR-based mutation testing is good for known mutations.
“Viruses mutate and especially RNA viruses like the coronavirus are more prone to undergoing mutations. As we now move from a pandemic to an endemic state, more and more people will either have the natural infection or will be vaccinated. As the human body mounts an immune response in either of those situations, there is selective pressure on the virus to mutate at higher rates. Recent data shows that the SARS-CoV-2 virus may be mutating much more rapidly that we may have anticipated. Some of these variants have been shown to be more transmissible. Some may impact the disease severity, and some may even impact vaccine efficacy. As the virus evolves, lab workers can expect to see certain variants harboring specific mutations becoming dominant in the population, a phenomenon called as convergent evolution,” explained Gandhi.
“Because there are so many mutations, labs really should consider their strategy to identify from strands,” Roberts added. “Think about how they want to tackle that issue to identify and report to the CDC or state labs to stay on top of mutations. It’s better for all of us Americans.”
References
- Centers for Disease Control and Prevention. 2021. COVID-19 and your health. Available at: https://www.cdc.gov/coronavirus/2019-ncov/transmission/variant.html. Accessed 1 April 2021.
- COVID-19 variant first found in other countries and states now seen more frequently in California | UC San Francisco. 2021. COVID-19 variant first found in other countries and states now seen more frequently in California. Available at: https://www.ucsf.edu/news/2021/01/419656/covid-19-variant-first-found-other-countries-and-states-now-seen-more. Accessed 1 April 2021.
- Center for Devices and Radiological Health. SARS-CoV-2 Viral Mutations: Impact on COVID-19 Tests. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/sars-cov-2-viral-mutations-impact-covid-19-tests?. Accessed April 6, 2021.
- New England Journal of Medicine. 2021. Serum neutralizing activity elicited by mRNA-1273 vaccine | NEJM. Available at: https://www.nejm.org/doi/full/10.1056/NEJMc2102179. Accessed 1 April 2021.
- Tom Pilgrim, P., 2021. New covid variant found in UK after 16 cases spark investigation. Daily Record. Available at: https://www.dailyrecord.co.uk/news/scottish-news/new-covid-variant-found-uk-23610523. Accessed 1 April 2021.
- Healthblog.uofmhealth.org. 2021. COVID Vaccines: Does it matter which one You get? Available at: https://healthblog.uofmhealth.org/wellness-prevention/covid-vaccines-does-it-matter-which-one-you-get. Accessed 1 April 2021
About the Author
Marisa L. Williams
Editor
The author of more than 100 independently published books, Marisa L. Williams earned her Master’s at Johns Hopkins University, while interning on Capitol Hill, doing press and communications for the National Association of Community Health Centers. Creating her own Bachelor of Science degree at the University of Toledo, Williams blended pre-medical, pre-law, and laboratory studies, resulting in an interdisciplinary degree emphasizing Forensics. She has worked with Dr. Paulette Moulton (Levy), a dermatologist in Monroe, MI, as well as Dr. Elizabeth Triana, a family medicine practitioner specializing in hormone therapy, based out of Port Charlotte, FL; additionally, she has 20 years of experience as a multimedia journalist, is a third generation Realtor licensed in MI and FL, and has five years of college level teaching experience.