Using laboratory analytics to improve performance in a value-based world of change
Laboratory administrators and department supervisors routinely manage supplies, perform risk assessments, and balance workloads and staffing. But managing these areas of operational performance has become even more challenging as laboratory administrators grapple with both the onslaught of COVID-19 testing and the healthcare industry’s move from fee-for-service to value-based reimbursement. For these reasons, making data-driven decisions based on laboratory analytics has become more important than ever to identify and manage change.
There are several issues that laboratory managers tackle on an hourly or daily basis. These include, but are not limited to, responding to requests for data, implementing new platforms for testing, and filling vacant positions. Not only are lab leaders faced with maintaining these and other routine day-to-day demands during the pandemic, but they must also sustain a competitive edge as a laboratory service.
As labs look inward and focus on addressing performance improvement and overall lab operations, there are many questions and challenges to successful daily management. Some of these include: Is our lab meeting turnaround times for all departments within the health system? Are we monitoring laboratory quality appropriately? How do we staff during a pandemic? What tests are being unnecessarily ordered? What follow-up tests are being missed? Where are we going to get our testing reagents, instruments, and supplies for molecular testing?
The answer to these questions resides in electronic data but accessing and interpreting data can be a time-consuming manual process. This is why laboratories are increasingly implementing solutions like laboratory analytics to automate and expedite this process and help with their daily management and process improvement effort.
Laboratory analytics brings data to your fingertips with reports that can be run ad hoc or scheduled when needed, allowing the laboratory managers to be in control of their data. By automating this process, which when done manually can take days or weeks, laboratory managers can make faster, actionable decisions on process improvement measures. Data management and analytics play a critical role in helping labs transition to value-based care by harnessing the power of data to improve operational efficiency, financial performance, and productivity.
Predicting workload with laboratory analytics software helps managers with staffing in uncertain times
Labs are always being asked to do more with less, and this is compounded by COVID-19 testing demands and financial strain caused by the pandemic. Laboratory staff members are overworked, stressed, tired, and concerned about COVID infections. Lab managers also deal with the possibility of staff furloughs, balancing and rotating staff by shifts, and sometimes working with skeleton crews.
Laboratory data analytics can help improve productivity by providing insight into staffing requirements based on several laboratory criteria. Analytics software allows the laboratory to monitor staffing needs by workstation, department, hours of the day, days of the week, by test, by patient location, and by priority. Once a user selects the criteria, lab analytics software can generate a report that displays by hour of the day where staffing adjustments may be necessary. Not only does this assist with staffing adjustments, but it also can help lab managers predict workload. Laboratory managers typically spend hours evaluating predictions of workload. Predictive workload reporting provides lab managers with views of how samples arrive on any given day of the week, by time, by any test or lab department. For example, predictive workload analytics provides lab management with the ability to view historical specimen arrivals by hour of the day and compare them to current arrivals to detect or predict new patterns. Using predictive analytics also can provide insights into making necessary staffing adjustments for phlebotomy and technical staff. If hematology specimen collections from intensive care units are now arriving 30 minutes earlier than previous Mondays, this would be a good indicator to have the early morning phlebotomy team members start their shift earlier. Predictive analytics also can be used to adjust staffing within the department. By viewing predictive analytics by hour of the day, any department can adjust technical staff as needed. Depending on the predictive workload by hour of the day, for example, they may decided to run quality control earlier or go to lunch later.
There are several opportunities to manage staffing levels with data analytics. One example is the ability to manage COVID-19 testing patterns and workflow by viewing the turnaround time (TAT) and frequency of batch COVID testing by hour and by shift. This is useful for monitoring interruptions in processing that cause turnaround time delays. It allows the laboratory to examine 24 hours of COVID-19 test processing at a glance by shift. The ability to view batch and frequency of COVID-19 testing data can assist laboratories in monitoring TAT, which is especially needed for high volumes of COVID-19 testing. The Lean ideal is Single Piece Flow, but this is not feasible for most COVID-19 testing platforms because COVID-19 instruments for hospital laboratories are typically designed for high batch-size processing. There are exceptions that support rapid, single piece flow. But the principal of smaller and more frequent batches will translate into decreased turnaround times. Smaller batches come at a cost of additional labor expended, so managers need to weigh the costs and benefits.1
Population heat maps also can be used to manage staffing. The heat maps reflect the volume of tests and positive COVID-19 results based on zip code and is used to identify high volume areas. This type of laboratory data management allows lab managers to predict staffing levels based on the increase of COVID-19 prevalence. Identifying areas becoming larger and darker on a heat map signals to management to prepare for changes in particular locations. As COVID-19 testing increases, decreases in routine testing will likely occur, which may impact staffing levels.
Improving test utilization for better financial performance during and beyond COVID-19
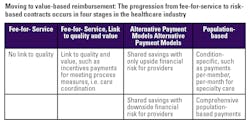
Over the last few years, laboratory reimbursements have declined and there has been a shift away from fee-for-service for inpatient testing, which has led to an increased emphasis on the quality and value of the services provided by clinical laboratories. With fixed reimbursement models no longer compensating for additional hospital clinical lab testing, and increased patient length of stays due to additional lab testing, test utilization has become one of the greatest opportunities for health systems to cut costs while improving patient outcomes and allowing them to meet the goals of value-based reimbursement models. (See Table 1)
Ultimately, the laboratory is sitting on a goldmine of data that has the potential to save the health system thousands or millions in unnecessary lab testing, which becomes increasingly important as value-based reimbursement becomes more commonplace. With data analytics, laboratory managers can independently generate reports to instantly identify sources of unnecessary testing. When the laboratory stewardship committee consults with physicians to eliminate these unnecessary tests or duplicate test orders, the cost savings are immediate. For example, hospital labs can reduce unnecessary inpatient sample collections by 6 percent, which provides an average $230k/year in cost avoidance (based on a hospital performing one million billable laboratory tests).2
Hospital laboratory analytics software enables laboratory management to monitor turnaround times to maximize reimbursement. The Centers for Medicare & Medicaid Services (CMS) announced that starting January 1, 2021, Medicare will pay $100 only to laboratories that complete high-throughput COVID-19 diagnostic tests within two calendar days of the specimen being collected. For laboratories that take longer than two days to complete these tests, Medicare will pay a rate of $75.3
Analytics can track turnaround times for COVID-19, regardless of testing location, such as tests that are sent out to state labs or completed in-house. This view into internal processes and any outliers that occur provides management with the data needed to both improve productivity and optimize financial performance by improving cost per test.
Conclusion
Managing patient and sample data with hospital laboratory analytics is an important way to get information immediately when needed. Laboratory leadership should not have to rely solely on IT for laboratory reporting, labs should have access to their data when they need it. The ability for lab managers to monitor the laboratory daily leads to improved operational and financial performance, saving valuable time for better quality and patient care. Hospital laboratory analytics software helps laboratory management monitor key performance indicators to lead their teams toward levels of best practices. In the end, laboratory analytics empowers the lab to become a hospital-wide partner and asset, while improving patient safety and satisfaction – during COVID-19 and beyond.
References
- Aretzweiler, G., Leuchter, S., Simon, C., Marins, E. and Frontzek, A., 2019. Generating timely molecular diagnostic test results: workflow comparison of the cobas 6800/8800 to Panther. Expert Review of Molecular Diagnostics, 19(10), pp.951-957. doi: 10.1080/14737159.2019.1665999.
- Visiun. Visiun.com. 2020. Test Utilization Module – Visiun. https://visiun.com/performance-insight/modules/test-utilization-module. Accessed October 30, 2020.
- CMS changes Medicare payment to support faster COVID-19 diagnostic testing. The Centers for Medicare & Medicaid Services. October 2020. https://www.cms.gov/newsroom/press-releases/cms-changes-medicare-payment-support-faster-covid-19-diagnostic-testing. Accessed October 29, 2020.
About the Author

Tim Bickley, MT(ASCP), MBA, CPHIMS
Is the Vice President of Sales, Visiun, Inc.