The clinical laboratory has long been accustomed to the need for quality assurance and quality control (QA/QC). For example, QC is routinely run on analyzers to safeguard against errant mechanical or assay performance; blood of known ABO types is regularly tested against reagents to ensure appropriate agglutination patterns; and known organisms are frequently used to confirm the proper growth and/or inhibitory characteristics of various growth mediums. The primary objective of these efforts is to guarantee, as well as possible, the accurate reporting of results that are vital to clinical decisions regarding the diagnosis and treatment of patients.
At the same time, in part due to an awareness of the nation’s challenges vis-à-vis healthcare costs, patients are increasingly considering their options for having their needs met with quality services that demonstrate value.1 This, in conjunction with evolving Medicare and Medicaid reimbursement models, has exerted a significant pressure on the healthcare sector, including the clinical laboratory. Accordingly, in an attempt to address rising costs and demonstrate value, laboratories are being compelled to expand their QA programs to include improvement initiatives that seek to enhance efficiencies.
Lean and the laboratory
Adopted from the Toyota production system, Lean (also known as synchronous manufacturing) is a philosophy that seeks to enhance efficiencies as a function of eliminating waste.2 Both value and an orientation toward the customer are central to this philosophy; therefore, in terms of Lean, waste refers to that which “consume[s] resources but from a customer’s perspective create[s] no value.”2 Based on this definition, there are seven types2 of waste that Lean attempts to mitigate; overproduction, inventory, waiting, unnecessary transport, unnecessary processing, unnecessary human motions, and defects.
In essence, the spirit of Lean endeavors is to “accomplish more with fewer resources.” To accomplish such, Womack and Jones, as cited by Meredith and Shafer,2 suggest that those aspiring to practice the tenets of Lean follow five principles. Indeed, when applied to the clinical laboratory, these principles, itemized below, can help crystalize both the vision and achievement of value:
Specify the customer’s perception of value. For clinical laboratories, the customer’s perception of value hinges on receiving accurate results in a timely fashion.
Recognize the value stream. The value stream for the laboratory includes the set of activities needed to collect, transport, and process specimens in such a way that accurate clinical and/or anatomic test results can be determined and provided back to the clinician.
Allow value to flow through the value stream. Value-adding activities include those actions needed to derive a result. Conversely, non-value adding, non-necessary activities include those actions that serve no purpose in value generation. Such activities include the rework necessary to address incorrectly ordered tests, instrument downtimes, and lost specimens. Mitigating these situations can streamline processes; effective pull communications (such as current procedure/test catalogs, etc.) can address the issue of incorrectly ordered tests; total productive maintenance can limit instrument downtimes; and visual aids that allow users to remain up-to-date with conditions in the lab can assist in preventing the loss of specimens.
Pull rather than push value through the value stream. The use of Kanban cards at the various benches within the labs can help pull value through the stream. As pull systems are control-based, specimens can be provided as the need exists rather than being pushed and potentially causing a backlog.
Continuously improve while seeking perfection. As situations improve in the medical laboratory, this should not present as an opportunity to claim success and resolve to implement Lean no further; instead, under the notion of continuous improvement, strides should be taken to find how processes can be further streamlined.
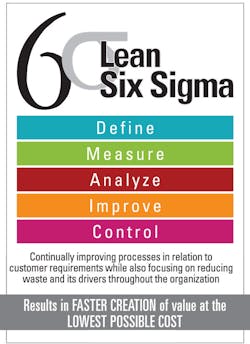
The case for Lean Six Sigma
Nevertheless, while Lean can serve to increase efficiencies as a function of eliminating waste in the form of non-value-adding work, it does not address another important element: inefficiencies created as a function of process variation. This is the role of Six Sigma. A concept developed in 1986 by then Motorola senior engineer Bill Smith, Six Sigma seeks to quantify process performance as a measure of variation. By identifying and remediating issues related to such variation, Six Sigma helps organizations, including clinical laboratories, achieve levels of process consistency.
Still, while organizations have certainly demonstrated the advantages and benefits associated with successfully implementing either Lean or Six Sigma, there has been a long-standing acknowledgement that either solution, when taken on its own merits, is not as effective as both methods taken together. Indeed, if only Lean were pursued, laboratories would, nevertheless, still need to contend with processes that may not be under statistical control while acceding to the notion that a scientific approach to quality, such as is found with Six Sigma, would be lost to initiatives solely utilizing Lean methodologies.3 Conversely, if only Six Sigma were used, a given initiative would be deprived of some of the benefits found in Lean,4 to include: a) being able to focus on increasing the speed of a process; b) being able to reduce the cost of inventories; and c) getting quick data, information, and/or results.
It stands to reason, then, that both Lean and Six Sigma are considered “excellent complements to each other”2 as the union of these methodologies yields an improvement process capable of applying Lean principles within a Six Sigma data-driven framework. Accordingly, Lean Six Sigma (LSS), as the name suggests, is the melding of Lean principles, as they regard the elimination of waste, with the data-driven statistical rigor of Six Sigma to reduce variation and develop consistency. This synergy helps bring about an even higher level of quality than can be attained by Lean or Six Sigma alone. Unfortunately, however, there currently exists no standard guidance in terms of integrating these approaches.5
Organizational culture and the success of Lean/LSS
Many clinicians as well as hospital administrators question whether data-driven improvement programs are applicable to the healthcare setting.6 This tendency to question the efficacy of improvement programs underscores what Albliwi et al refer to as a “resistance to culture change.”7 Indeed, the extent to which Lean can be successfully adopted by any organization, including laboratories, is fundamentally dependent upon the culture of that organization.8
With this in mind, it is fair to suggest that these improvement methodologies cannot be formulated simply as a set of tools, practices, and techniques, for without an organizational culture supportive of exerting the effort necessary to adopt Lean principles, the improvement initiative may flounder. Instead, for organizations aspiring toward QA initiative success, these improvement methodologies necessitate both broad commitment and a holistic approach that requires “a systematic and controlled strategy to look at the prevailing culture.”8 If a variance between the current culture and the targeted cultural condition is identified, then it is incumbent upon management to enact the embedding mechanisms needed to align the culture with the strategic vision. This is not outside the realm of management’s responsibility; indeed “perhaps the most important mission of a manager is the adjustment of the organizational strategy in the area of culture.”9
The business benefits of Lean/LSS deployment
The benefits2 of Lean include reduced costs, increased revenues, greater employee morale and engagement, and better quality and processes. Additionally, for those able to successfully leverage LSS, the benefits5 include an increase in available capacity, increased productivity for staff, and increased accuracy of laboratory result data. With this in mind, and given the economic uncertainty of today’s healthcare environment, the need to do more with less while demonstrating one’s value proposition is integral to long-term sustainability. Accordingly, a potential competitive advantage awaits those medical laboratories and other healthcare organizations capable of successfully implementing Lean/LSS.
REFERENCES
- D’Souza S, Sequeira AH. Measuring the customer-perceived service quality in health care. Journal of Health Management. 2012;14(1):27-41. doi:10.1177/097206341101400103.
- Meredith JR, Shafer SM. Operations Management for MBAs. 5th ed. Hoboken, NJ: John Wiley & Sons, Inc; 2013. pages 171-181,197,198.
- Assarlind M, Gremyr I, Bäckman K. Multi-faceted views on a Lean Six Sigma application. International Journal of Quality & Reliability Management. 2012;29(1):21-30. doi:10.1108/02656711211190855.
- Atmaca E, Girenes SS. Lean Six Sigma methodology and application. Quality & Quantity. 2013;47(4):2107-2127. doi:10.1007/s11135-011-9645-4.
- Ahmed S, Manaf NHA, Islam R. Effects of Lean Six Sigma application in healthcare services: a literature review. Reviews on Environmental Health. 2013;28(4):189-194. doi:10.1515/reveh-2013-0015.
- DelliFraine JL, Wang Z, McCaughey D, Langabeer JR, Erwin C. The use of Six Sigma in health care management: are we using it to its full potential? Quality Management in Health Care. 2014;23(4):240-253. doi:10.1097/QMH.0000000000000039.
- Albliwi S, Antony J, Lim SAH, Wiele T. Critical failure factors of Lean Six Sigma: A systematic literature review. International Journal of Quality & Reliability Management. 2014;31(9):1012-1030. doi:10.1108/IJQRM-09-2013-0147.
- Bhasin S. Impact of corporate culture on the adoption of the Lean principles. International Journal of Lean Six Sigma. 2013;4(2):118-140. doi:10.1108/20401461311319329.
- Hosseini SA. Components of organizational culture based on Denison model. Kuwait Chapter of Arabian Journal of Business and Management Review. 2014;3(12a):31-42. http://www.liberty.edu:2048/login?url=http://search.proquest.com.ezproxy.liberty.edu:2048/docview/1553534862/fulltextPDF?accountid=12085.
Lynn Hamilton, MBA, PMP, MLT(ASCP), serves as Manager, Laboratory Systems Engineering, University of Virginia Health System, where he is responsible for both the daily administration of staff providing IT support for operations throughout the medical laboratories and the project management of lab-related IT initiatives.