Latest studies by Boston Medical Center have revealed that individuals who live with HIV and have previously experienced pulmonary tuberculosis develop a more robust and broader HIV antibody reaction, as well as a higher likelihood of having HIV sequences that are expected to be resistant to antibodies, compared to those who have no history of suspected or recorded tuberculosis. The research, which was published in iScience, indicates that coexisting tuberculosis has a significant influence on the immune responses to HIV and the viruses that are prevalent in HIV-positive individuals.
The research findings suggest that tuberculosis could affect the effectiveness of antibody-based prevention and therapeutic approaches for HIV. Vaccines that stimulate the production of antibodies and antibodies themselves are being explored as potential treatments and cures for HIV. However, the higher occurrence of antibody-resistant strains, coupled with the presence of tuberculosis, implies that such antibody-based interventions are more likely to fail in affected individuals.
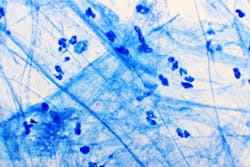
The research team collaborated closely with investigators in Uganda and the AIDS Clinical Trial Group (ACTG) to gather samples from people who were recently diagnosed with HIV, with or without tuberculosis. Samples were obtained from these individuals both prior to and about six months after initiating HIV medication. The team compared antibodies, plasma inflammatory markers, and HIV sequences in the baseline and treatment samples to determine any differences.
The study found that tuberculosis disease is linked to a higher prevalence of some antibody-resistant strains of HIV. In regions of the world where tuberculosis is common and HIV transmission is ongoing, the presence of these antibody-resistant strains suggests that a potential vaccine that stimulates the production of broad and potent antibodies may not be effective.