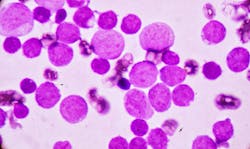
Breakthrough studies in hematopathology — including advances in genetic testing, relapse prediction and detection of hidden, disease-defining gene fusions in AML — were presented at the Association for Molecular Pathology (AMP) 2025 Annual Meeting & Expo.
Below are just a few of the hematopathology findings that will be shared by leading experts in molecular diagnostics at AMP 2025:
- Genetic testing could help predict relapse after stem cell transplant: A University of California San Diego study suggests that genetic testing after stem cell transplant may help identify patients who are most likely to relapse. Researchers reviewed data from 74 patients and used next-generation sequencing to track cancer-related gene mutations at three points: at diagnosis, after chemotherapy and after transplant. They found that lingering mutations after transplant strongly predicted relapse, particularly in the TET2 and DNMT3A genes. By contrast, patients whose donor cells successfully took over the bone marrow often remained cancer-free — even if tests still picked up very low-level genetic changes, which may reflect harmless background mutations rather than leukemia.
- New testing method improves detection of hidden genetic drivers in AML: Researchers at the University of Michigan added an RNA-based fusion test to their standard next generation sequencing panel for myeloid cancers. Reviewing more than 600 AML cases, they found gene fusions in 15% of patients, including 23 cases (about 4% of all AML samples) where the fusion was missed by conventional cytogenetics. These included important rearrangements involving genes such as NUP98 and KMT2A, which can alter treatment approaches. The findings show that incorporating RNA-based fusion testing into routine AML diagnostics can reveal hidden, disease-defining gene fusions that otherwise would go undetected, ensuring patients receive a more accurate diagnosis and the most appropriate treatment.
- New sequencing test improves detection of residual cancer: Scientists at Moffitt Cancer Center have validated a highly sensitive genetic test to track residual disease in patients with AML. The test focuses on changes in the FLT3 gene, which are common in AML and linked to higher relapse risk. Detecting even tiny traces of these mutations can help doctors confirm remission, decide whether a patient should have a stem cell transplant, and intervene earlier if the cancer is returning. Using deep sequencing, the team showed the test could find FLT3 mutations at extremely low levels — down to 0.0014% — with strong accuracy and reproducibility. These results support the test as a powerful tool for monitoring patients after treatment, giving clinicians greater confidence in disease status and enabling more timely treatment decisions.
About the Author
Sign up for our eNewsletters
Get the latest news and updates