A method of testing for prostate cancer developed at the National Cancer Institute (NCI) leads to more accurate diagnosis and prediction of the course of the disease, according to a large study. This method, which combines systematic biopsy, the current primary diagnostic approach, with MRI-targeted biopsy, is poised to greatly improve prostate cancer diagnosis, thereby reducing the risk of both overtreatment and undertreatment of the disease. NCI is part of the National Institutes of Health.
The findings were published March 5, 2020, in the New England Journal of Medicine. The study was conducted at the NIH Clinical Center in Bethesda, Maryland.
“Prostate cancer has been one of the only solid tumors diagnosed by performing systematic biopsies ‘blind’ to the cancer’s location. For decades this has led to the overdiagnosis and subsequent unnecessary treatment of non-lethal cancers, as well as to missing aggressive high-grade cancers and their opportunity for cure,” said Peter Pinto, MD, of the Urologic Oncology Branch in NCI’s Center for Cancer Research and senior author of the study. “With the addition of MRI-targeted biopsy to systematic biopsy, we can now identify the most lethal cancers within the prostate earlier, providing patients the potential for better treatment before the cancers spread.”
Prostate cancer can vary widely in severity and its potential to spread. Low-grade prostate cancer is associated with a very low risk of cancer-specific death and often doesn’t require treatment, whereas high-grade cancers are much more likely to spread and are responsible for most prostate cancer deaths. This makes the correct assessment of the cancer grade very important for treatment decisions.
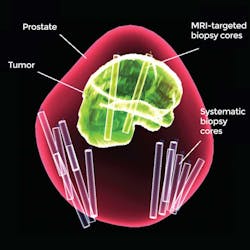
Unlike biopsies for most other types of cancer, which target abnormalities found by imaging, systematic biopsy uses a non-targeted method of taking systematically spaced samples across the prostate gland to find a cancer. Because this method can potentially miss areas of cancer, doctors may then overtreat a patient with low-grade disease, fearing there is high-grade disease they missed. Or, if an aggressive cancer is missed, a patient may be undertreated.
MRI-targeted biopsies, which merge previously taken MRI images of suspected cancer with real-time ultrasound technology, are better able to detect more high-grade cancers than systematic biopsies. The goal of this study was to determine whether it would be better to replace systematic biopsy with MRI-targeted biopsies or use both tests together.
In the study, 2,103 men who had MRI-visible lesions underwent both MRI-targeted and systematic biopsies. Of these men, 1,312 were diagnosed with cancer and 404 underwent prostatectomy, a full removal of the prostate. By comparing diagnoses from systematic biopsy alone to systematic biopsy plus MRI-targeted biopsy, the researchers found that adding MRI-targeted biopsy to systematic biopsy led to 208 more cancer diagnoses than systematic biopsy alone. The addition of MRI-targeted biopsy also led to 458 upgrades, or changes in diagnosis to a more aggressive cancer, based on analysis of the biopsy tissue by histopathology.
The researchers also determined that combined biopsy provided more accurate diagnosis than MRI-targeted biopsies alone. Among the men who underwent prostatectomy, the researchers found that systematic biopsy alone underdiagnosed about 40 percent and MRI-targeted biopsy alone underdiagnosed about 30 percent of the cancers, while combined biopsy underdiagnosed 14.4 percent of the cancers. In addition, while systematic biopsy underdiagnosed 16.8 percent and MRI-targeted biopsy underdiagnosed 8.7 percent of the most aggressive cancers, combined biopsy missed only 3.5 percent of the most aggressive cancers.
MRI-targeted biopsies were first developed more than 10 years ago by a team of NCI researchers led by Dr. Pinto; Bradford Wood, MD; Baris Turkbey, MD; and Peter Choyke, MD, all co-authors of the new study. The team, which included other researchers from NCI and other organizations, worked with Philips Healthcare to develop software that could overlay MRI images onto ultrasound images in real time, providing a view of lesions to be sampled that’s not possible with systematic biopsy.