CDC study highlights need for ongoing monitoring to identify emergence of antibiotic-resistant bacteria in community settings
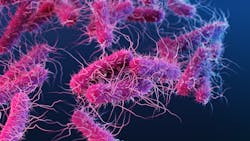
A study led by researchers at the U.S. Centers for Disease Control and Prevention (CDC) suggests that ongoing population-based surveillance is critical to monitor for the emergence of carbapenem-resistant Enterobacterales (CRE) outside of traditional healthcare settings.
Published in the American Journal of Infection Control (AJIC), the study found that a small but notable proportion of CRE cases, a type of bacteria that can cause severe and difficult-to-treat infections, occurs in individuals who are not known to have traditional healthcare risk factors.
CRE are an important cause of multidrug-resistant infections and can spread rapidly, contributing to their classification by CDC as an urgent U.S. public health threat. Additionally, some CRE produce a carbapenemase gene that can be shared between different bacteria, accelerating the spread of resistance and the risk for hard-to-treat infections. Traditionally, patients that become infected with CRE have an ongoing healthcare exposure or a history of it, such as hospitalizations or stays in long-term care facilities. However, cases of CRE without healthcare risk factors have emerged in recent years. The study published represents the first population-level description of such community-associated (CA) CRE in the United States.
“While only 10% of the CRE cases in our study were determined to be community-associated, this finding, coupled with the fact that five of 12 CRE isolates we sequenced had carbapenemase genes is concerning,” said Sandra Bulens, MPH, health scientist in CDC’s Division of Healthcare Quality Promotion, and lead author on the study. “Further investigation is needed to understand this emergence in the community and how infection prevention and control efforts can be targeted to reduce spread.”
Previous reports have suggested that international travel, previous antibiotic use, or contact with family members who frequently receive treatment or visit healthcare facilities may play a role in CA-CRE cases.
The current study used data obtained from eight U.S. metropolitan areas between January 2012 and December 2015 as part of CDC’s Emerging Infections Program (EIP) Healthcare-Associated Infections – Community Interface Activity, which has conducted laboratory- and population-based surveillance for CRE and other drug-resistant gram-negative bacteria since 2011. Researchers identified patients diagnosed with CRE, and then compared the incidence and epidemiology of CA-CRE cases to CRE cases with healthcare risk factors. Cases were classified as CA-CRE if they had no known healthcare risk factors, based on medical record review, and a culture collected <3 days after hospital admission.
In total, researchers identified 1,499 CRE cases among 1,194 patients with documented CRE. Among these, 149 CRE cases (10%) were classified as community associated. The incidence of CRE cases per 100,000 population was 2.96 (95% CI: 2.81, 3.11) overall and 0.29 (95% CI: 0.25, 0.25) for CA-CRE. Most CA-CRE cases were in White persons (73%) and females (84%).
As part of the study, researchers performed whole genome sequencing on a subset of CRE isolates. Among the 12 sequenced CA-CRE isolates, 5 (42%) harbored a carbapenemase gene. Preventing the spread of these carbapenemases is critical because they are resistant to some newer antibiotics.