Detection of Group B streptococcus in the clinical laboratory
Streptococcus agalactiae, also known as Group B strep (GBS), is a Gram-positive colonizing bacterium that can cause life-threatening complications for newborns when it is passed to them from their mothers. This bacterium has been found in as many as 30 percent of healthy women,1 to whom it poses little danger. According to the American Pregnancy Association, Group B strep is found in as many as one in every 2,000 children born in the United States each year.2
Women in the last few weeks of pregnancy are frequently tested for GBS due to the possibility of transmitting the bacteria to a newborn baby. Through screening, clinicians identify whether the baby may be at potential risk. Clinical laboratory professionals frequently test microbiology samples specifically for Streptococcus agalactiae. By utilizing established screening testing of late-term mothers, laboratory professionals assist obstetrical physicians in identifying potential threats to newborns, as well as their mothers.
The threat of Group B strep
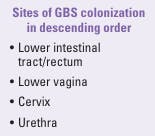
Group B strep infection does not pose a considerable threat to the mother, but the organism may profoundly impact the health of a newborn. Presentation of GBS infection in the mother is typically found in the rectum/ lower intestinal tract and secondarily in the vaginal tract. See Figure 1 for the common sites of GBS colonization. The most common treatment is penicillin or ampicillin; in some cases, increased resistance to antibiotics have been noted. In addition, a recent study found “increased odds of MRSA carriage in GBS positive women.”1 The CDC recommends vaginal GBS screening of all women in the late stages of pregnancy.2 (Non-pregnant adults who are immunocompromised due to cancer, diabetes, HIV, or increased age are also at-risk for GBS infection development.3)
GBS bacteria come and go naturally in people's bodies. People may test positive for the bacteria at some times and not others. That's why women get tested late in their pregnancy, close to the time of delivery. Hence, the purpose of screening pregnant women from 35 to 37 weeks gestation is to identify possible GBS infection for the mother and also to give an indication of the possibility that the newborn could be infected at the time of birth. Infection can occur either while the child is still in the placenta or during birth. Risk factors for neonatal GBS include prenatal colonization, premature delivery, prolonged rupture of membranes, intrapartum fever, and a prior baby with GBS.
Onset of neonatal disease is characterized by several possible health complications; however, the most common pathogenesis is meningitis. Meningitis symptoms can include fever, lack of appetite, excessive crying, vomiting, and a bulging soft spot (fontanelle). Other possible infections include sepsis (infection of the blood), pneumonia (infection of the lungs), skin and soft tissue infections, and bone and joint infections.4
Meningitis and sepsis in newborns can result in an increased mortality rate depending on complications and the child’s susceptibility to antibiotic resistance.
According to Chen et al, prior to the introduction of GBS screening in pregnant mothers, “GBS was responsible for substantial perinatal morbidity and mortality, with as many as one to three in 1,000 neonates affected.”3 Development of symptoms of GBS infection during the first six days of life is called early onset; development of symptoms between seven days and three months is called late onset.5 The addition of antibiotics to GBS-colonized women prior to the child’s birth has led to a decrease in mortality rates, from >50 percent in the 1970s to <10 percent by the 1990s.”3 However, GBS remains a significant cause of both neonatal bacterial meningitis and sepsis.”3 Testing by the clinical laboratory thus remains critical to bacterial identification and early prevention of transmission to the newborn child.
Laboratory testing approaches
In 2021, the American Society for Microbiology (ASM) released new guidelines for detecting and identifying GBS to prevent disease in newborns.6 The GBS culture technique remains the gold standard. Nucleic acid amplification tests (NAAT) alone are not as sensitive and can produce false negatives. However, a modified testing technique that utilizes the broth enrichment step first increases sensitivity of NAAT.
A brief description of the ASM guidelines is as follows:
· Use selective enriched broth that enhances growth of GBS. Incubate for 18–24 hours, 35–37 degrees.
· Culture media and GBS isolation methods should detect both hemolytic and non-hemolytic strains.
· Report GBS in any quantity from urine cultures from pregnant women during all trimesters.
· Acceptable phenotypic and proteomic methods of identification of candidate isolates include CAMP test, latex agglutination, and MALDI.
· Nucleic acid amplification–based identification of GBS from enrichment broth is acceptable, but not sufficient for all patients.
· Latex agglutination directly from enrichment broth and direct-from-specimen immunoassays are unacceptable methods for GBS detection.
· Perform antimicrobial susceptibility testing on all GBS isolates from pregnant women with penicillin allergy. For those without a known penicillin allergy, antimicrobial susceptibility testing is not required but should still be considered.
Conclusion
Laboratory testing for GBS has not changed significantly over the past decade and culture remains the gold standard method. However, disadvantages of culture are prolonged incubation and not allowing for point-of-care testing. Molecular methods from enrichment broth culture for GBS detection and identification are routinely used today. The shortened turnaround time of about an hour after broth enrichment allows timely administration of appropriate antibiotic therapy for GBS positive patients.
References
- Parriott AM, Brown JM, Arah OA. Predischarge postpartum methicillin resistant Staphylococcus aureus infection and group B streptococcus carriage at the individual and hospital levels. Infect Dis Obstet Gynecol. 2014;2014:515646. doi:10.1155/2014/515646.
- Group B Strep Infection: GBS. American Pregnancy Association. Accessed May 22, 2025. http://americanpregnancy.org/pregnancy-complications/group-b-strep-infection/.
- Chen VL, Avci FY, Kasper DL. A maternal vaccine against Group B streptococcus: past, present and future. Vaccine. 2013;31 Suppl 4:D13-9. doi:10.1016/j.vaccine.2012.12.080.
- Puopolo KM, Lynfield R, Cummings JJ. Committee on Fetus and Newborn, Committee on Infectious Diseases. Management of infants at risk for group B streptococcal disease. Pediatrics. 2019;144(2):e20191881. doi:10.1542/peds.2019-1881.
-
Group B streptococcal septicemia of the newborn. MedlinePlus. Updated November 5, 2022. Accessed May 22, 2025. https://medlineplus.gov/ency/article/001366.htm.
- Guidelines for the detection and identification of Group B Streptococcus. ASM. Updated July 23, 2021. Accessed May 22, 2025. https://asm.org/guideline/guidelines-for-the-detection-and-identification-of.
This article was originally published in MLO's July 2015 issue. It was updated in 2025 by Christina Wichmann.
About the Author

Lt Col Paul R. Eden, MT(ASCP), PhD, USAF (retired)
has 24 years of laboratory experience managing both clinics and hospital laboratories including over six of years of applied research. He is also serving as Adjunct Assistant Professor, Pharmacology & Toxicology, Wright State University, Ohio.