The need for earlier detection and reliable intervention monitoring for managing sepsis
Remarkably resilient in protecting against disease, the wonders of the human body inspire medical scholars and nascent students alike. But when immune responses overreact to infection, a dangerous process begins, potentially resulting in organ damage and even death.
Sepsis, regarded as the number one cause of preventable death worldwide, garners nearly 49 million cases and 11 million deaths annually, representing approximately 20% of global fatalities.1 In the United States, at least 1.7 million adults contract sepsis every year.2 Of this population, 350,000 will die in the course of care, accounting for approximately one third of national hospital deaths.2 Sepsis remains a critical global concern, but advances in microbiology research and diagnostics are helping advance earlier intervention to help improve patient outcomes.
In alignment with the second strategic pillar of the 2030 Global Agenda for Sepsis, a key element in reducing this critical risk is health system investment in education, training, and tools to prevent adverse patient outcomes.4 This initiative begins with adopting robust early detection and active monitoring measures.
A story of sepsis survival
Despite far-reaching advances in clinical delivery, sepsis remains a formidable medical challenge due to both its rapid onset and lack of awareness. Individuals who acquire sepsis require urgent intervention as treatment delays set the stage for often irreversible bodily harm and heightened mortality risks.
This is a truth I know all too well due to my own near-fatal experience with this infection.
In 2024, after having routine thyroid surgery, I spent the next 24 hours in a medically induced coma as physicians attempted to subdue a rapidly spreading infection that took hold in my upper body. After three procedures to remove the tissues damaged by necrotizing fasciitis, I learned that the infection spread to my abdomen—a disheartening prognosis for me and my loved ones. Fortunately, I was administered antibiotics that helped fight off the infection, reversing an ill-fated trajectory.
In my case, the first signs of sepsis occurred only hours after I was discharged from surgery. My recovery is attributed to the timely action of clinicians who accurately recognized my symptoms and quickly routed me to a larger hospital skilled in treating serious infections.
Other patients are not as fortunate. Across the world, early symptoms are much too often ignored or attributed to less severe illnesses. When sepsis enters the equation, timely treatment is not only a medical best practice, but a matter of survival.
The imperative for early detection
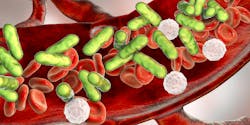
Sepsis occurs when infection enters the bloodstream triggering mass inflammation. In its most advanced stages—septic shock—with every hour of delayed treatment, a patient’s risk of mortality increases by 8%.5
Early detection is key to preventing adverse patient outcomes, as it paves the way for prompt, life-saving treatment, reducing the risk of organ failure, necrosis, and death. However, in resource-constrained settings, such as emergency rooms or intensive care units, clinicians have a limited number of methodologies to accurately identify sepsis at the point of care.
Current clinical evaluation protocols, including the systemic inflammatory response syndrome (SIRS) criteria, provide a starting point to identify common sepsis indicators. However, to confirm sepsis using this protocol, symptoms must meet SIRS criteria and microbial infection must be highly suspected or confirmed through laboratory testing. The quick Sequential Organ Failure Assessment (qSOFA) is similarly an initial screening tool to identify patients who meet sepsis risk criteria. This tool has notable drawbacks due to limited diagnostic sensitivity in select patient populations.6
The accuracy and flexibility challenges of sepsis screening tools underscore the need for faster, reliable diagnostic solutions for versatile care settings.
Reliable monitoring: The role of laboratory medicine
Leading diagnostic tools are fundamental to both the early identification and ongoing management of sepsis. These tools complement clinical evaluations, enabling more objective assessments.
Biomarkers like procalcitonin (PCT), serum lactate, and MR-proADM have proven utility in detecting clinically relevant bacterial infections and determining infection severity. PCT testing is a powerful intervention for not only revealing the level of infection found in the body, but informing treatment decisions, such as antibiotic administration.
Using PCT, clinicians can determine whether administered antibiotics are effective at combating infections and how long to continue antibiotic treatment. Research suggests that daily PCT testing may significantly reduce antibiotic treatment duration in sepsis patients compared to standard care protocols.7 In a time of rising antimicrobial resistance (AMR), PCT deters antibiotic overuse advancing antibiotic stewardship.8 Additional clinical benefits from decreased antimicrobial exposure include reduction in adverse drug events, C. difficile infections, 30-day readmissions, length of hospital stay, and hospital costs.
Microbiology testing methodologies, such as culture media, are also central to effective sepsis management. Utilizing prepared media, medical laboratory professionals can grow microbial colonies from positive blood samples and subsequently identify the specific pathogen(s) present. After pathogen identification, antimicrobial susceptibility testing (AST) is performed on the isolated colonies to determine the lowest concentration—minimum inhibitory concentration (MIC)—of antimicrobials that inhibit microorganism growth.
AST guides the selection of the most effective antibiotic to treat infections, and in doing so, may also identify antimicrobial resistance. These methods inform more precise diagnoses and targeted therapies. Additionally, molecular diagnostics, including PCR (polymerase chain reaction) tests, make rapid, accurate pathogen identification possible with a high degree of sensitivity.
With biomarker testing paired with clinical microbiology solutions, clinicians are equipped with the tools to increase diagnostic accuracy, accelerate care, and monitor treatment responses—all key to optimizing clinical delivery and transforming sepsis patient outcomes.
Systemic change and cross-disciplinary collaboration
In sepsis management, the role of microbiology is not limited to individual diagnoses. From guiding disease control initiatives to informing antimicrobial stewardship, clinical microbiology influences all levels of the infection management continuum. This link between microbiology and clinical care points to an integral element of sepsis management: cross-disciplinary collaboration.
Clinicians can administer care at the highest level when equipped with reliable, accurate tools to augment clinical judgement and complement manual evaluations. In effect, close collaboration between microbiologists and laboratory management professionals ensures that point-of-care insights inform diagnostic development and likewise, microbiology discoveries enhance clinical care.
As the global medical community seeks to combat rising sepsis rates, collaboration between microbiology and medical laboratories will also strengthen health system investment in sepsis prevention and detection measures. These measures, formalized in the 2021 Surviving Sepsis Campaign (SSC) guidelines, include standardized screening protocols for high-risk patients, rapid diagnostic testing for suspected infections, and as advised, immediate administration of antimicrobials following diagnosis.9 Leveraging the latest diagnostic insights, hospitals, health systems, and emergency care facilities also have an opportunity to incorporate sepsis awareness into ongoing patient education and public health initiatives.
The cumulative effect of collaboration is one of continuous improvement. When clinicians, laboratory management professionals, and microbiologists engage around latest findings and best practices, the need to track infection rates, compliance metrics, and patient outcomes is even more pronounced. Cross-disciplinary collaboration is essential to the widespread adoption of sepsis prevention and management protocols, as well as diagnostic innovation and quality care.
The path forward
As a sepsis survivor, I know firsthand how quickly a bacterial infection can escalate into a dire emergency. For both myself and patients around the world, early detection of infection and active monitoring of sepsis symptoms made the difference between life and death.
While there are countless challenges in healthcare that often appear insurmountable, combatting the rise of sepsis is one goal that is well within reach.
Through the dissemination of new findings and sharing of best practices, collaboration between medical laboratories and microbiology partners is instrumental to lowering sepsis incidence globally. Further, by integrating diagnostic tools and microbiology testing with clinical evaluation, clinicians are empowered with a robust toolkit to manage sepsis in a variety of care settings.
When we shift our focus to view early identification and active monitoring of sepsis as a critical priority, rather than an afterthought, we provide patients with not only the best chance of recovery, but another shot at life.
REFERENCES
- Sepsis. World Health Organization. May 3, 2024. Accessed August 29, 2025. https://www.who.int/news-room/fact-sheets/detail/sepsis.
- About sepsis. Centers for Disease Control and Prevention. August 19, 2925. Accessed August 29, 2025. https://www.cdc.gov/sepsis/about/index.html#:~:text=Quick%20facts,23.
- Morrissey R, Lee J, Baral N, et al. Demographic and regional trends of sepsis mortality in the United States, 1999-2022. BMC Infect Dis. 2025;25(1):504. doi:10.1186/s12879-025-10921-7.
- The 2030 global agenda for sepsis. Global Sepsis Alliance. Accessed August 29, 2025. https://globalsepsisalliance.org/2030-global-agenda-for-sepsis.
- McGregor C. Improving time to antibiotics and implementing the "Sepsis 6". BMJ Qual Improv Rep. 2014;2(2):u202548.w1443. doi:10.1136/bmjquality.u202548.w1443.
- Kim KS, Suh GJ, Kim K, et al. Quick Sepsis-related Organ Failure Assessment score is not sensitive enough to predict 28-day mortality in emergency department patients with sepsis: A retrospective review. Clin Exp Emerg Med. 2019;6(1):77-83. doi:10.15441/ceem.17.294.
- Dark P, Hossain A, McAuley DF, et al. Biomarker-guided antibiotic duration for hospitalized patients with suspected sepsis: The ADAPT-sepsis randomized clinical trial. JAMA. 2025;333(8):682-693. doi:10.1001/jama.2024.26458.
- Antimicrobial resistance facts and stats. Centers for Disease Control and Prevention. February 4, 2025. Accessed August 29, 2025. https://www.cdc.gov/antimicrobial-resistance/data-research/facts-stats/index.html.
- Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063-e1143. doi:10.1097/CCM.0000000000005337.
About the Author

Jeroen Bursens, Sr.
is a Senior Scientific Affairs Manager at Thermo Fisher Scientific. With over 25 years of experience in specialty diagnostics and clinical microbiology, Jeroen is an advocate for public health education and awareness.