RT-PCR usage expands as preferred method of infection detection
Within clinical labs, rapid reverse transcription polymerase chain reaction (RT-PCR) tests have become standard protocol due to their speed and sensitivity in diagnosing cases of infection such as influenza and Strep. More recently, however, the same test features are being relied upon for a different best practice application – detecting cases of global infections, which have seen the tests’ usage increase on par with diagnosed patients.
Traditional clinical use
Since its introduction to the clinical lab industry, RT-PCR (also known as qPCR – quantitative polymerase chain reaction) found its place as a reliable and reproducible method of infection detection. Looking at its top applications, John Osiecki, PhD, Director, Medical and Scientific Affairs, Molecular Diagnostics at Roche Diagnostics Corporation, said, “PCR has a diverse array of applications. With the capability of detecting single copies of the genetic signature of pathogens in human samples, it has been a critical tool in clinical diagnostics for infections such as influenza, Group A Streptococcus, Chlamydia and Gonorrhoeae.”
He added, “Due to its ability to accurately quantify the presence of pathogens in blood, PCR technology has provided physicians with confidence to manage patients across different therapeutic regimens for chronic infections such as HIV and Hepatitis C, and even alert physicians to rising amounts of Human Cytomegalovirus in patients following transplant.”
When asked about some of the industry trends in PCR usage, and why it’s preferred, Osiecki replied, “PCR is exquisitely sensitive and very specific, which promotes confidence as a ‘go to’ tool for the laboratory. The industry is shifting toward adoption of PCR protocols with a dual-target approach, allowing a level of redundant coverage by detecting two different genes in a specific bacterium or virus. As these pathogens evolve due to error-prone processing of their own genetic material, or selective pressure from a variety of therapeutic treatments, the PCR diagnostic tools maintain excellent performance.”
As the use of RT-PCR increases, market researchers predict an aggressive growth rate. According to research firm MarketsandMarkets, “the global dPCR (digital PCR) and qPCR market is projected to reach USD 6.3 billion by 2024 from USD 4.1 billion in 2019, at a CAGR of 8.8 percent from 2019 to 2024.” Cited as the primary driving force for the growth of this market is the “rising incidences of target diseases and genetic disorders, increasing use of biomarker profiling for disease diagnostics and continuous technological advancements in PCR technologies,” among other factors.1
Best choice options
Looking at the advantages and any apparent limitations of using RT-PCR versus other clinical options, Osiecki pointed out, “Sensitivity, specificity and confidence in reporting are the real strengths of PCR technology. Most applications include internal controls that are processed simultaneously with the target, helping us to know a true sample was present and the process worked as it should.”
He continued, “Every method has limitations, and one of the primary concerns in the early days of PCR was the risk of contamination. The process involves amplifying tremendous amounts of target sequence of interest, and open systems could spread this amplicon to the laboratory environment, potentially generating false positives for new samples that were exposed. Design features such as closed systems where the amplification is detected through the wall of a completely sealed reservoir have minimized this risk. Also, the addition of enzymes that selectively degrade any residual amplicon from previous PCR runs, such as uracil N-glycosylase, has been shown to be effective.”
RT-PCR as cost-effective choice
When it comes to fast and accurate infection detection, RT-PCR seems the logical choice for clinicians, but at what cost? MarketsandMarkets points out that “a typical PCR analysis conducted through dPCR instruments involves several scientific technologies (PCR, microfluidics, and nanofabrication) integrated to achieve the desired process outcome. These instruments are small and boast reduced cycle times. However, the development of such instruments requires large capital investments and extensive scientific validation on a nanoscale level.”1
Adding to the capital investment is that because “dPCR is a relatively new technology; as a result, most manufacturers often price their state-of-art dPCR instruments at a premium (~USD 120,000) compared to qPCR instruments (~USD 50,000). For instance, as of January 2016, the average price of a dPCR instrument is reported to be USD 55,000–120,000, according to their device architecture and target application area in the U.S.”1
But for people like Osiecki, the benefits far outweigh any associated costs of using RT-PCR tests. “Traditionally, bacterial and viral culture for identification of pathogens was labor intensive and could take days. PCR technology has improved the turnaround time dramatically, and newer applications include fully automated sample processing, amplification and detection. Taken together, PCR applications can improve lab efficiency by allowing our highly skilled laboratory professionals to focus on other tasks,” he said.
When considering the actual cost of RT-PCR tests, a simple internet search shows figures as low as $15-25 per test to amounts in the hundreds for more detailed and extensive tests. However, these amounts are often overlooked when compared with the higher costs associated with tests that are not as fast or reliable, do not offer early detection and have the patient suffer much longer than necessary.
Future usage grows
Looking to the future of RT-PCR clinical lab usage as additional options for DNA/RNA analyses become available, Osiecki said, “There are many new applications for PCR technology that will benefit the clinical community in the years to come. For example, new diagnostic tests are being developed for applications in transplant for monitoring the presence of EBV and BK Viruses, where FDA-approved solutions were not available in the past.”
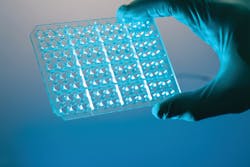
He added, “New systems are being introduced that provide laboratory-quality results with PCR technology in 20 minutes or less with a point-of-care (POC) device. Digital PCR, a method that captures nucleic acids and separates them into tiny wells for individual PCR reactions, can provide unprecedented accuracy in absolute quantification, monitoring of cancer by evaluating liquid biopsies, and rare mutation detection of one in 200,000 of wild type background.”
According to forecasted statistics from MarketsandMarkets, North America is expected to account for a large amount of RT-PCR growth during the 2019-2024 time period. In addition, a recent global event has created the need for a significant increase in RT-PCR test usage in Asia-Pacific countries, unfortunately.1
Global best practices
While the clinical lab industry has busied itself with infection detection within the lab environment, another best practice use for RT-PCR testing was created when a new virus emerged in Wuhan, China, in December 2019. The novel coronavirus, referred to as COVID-19, has demonstrated the efficiency and efficacy of using RT-PCR testing by way of thousands of suspected cases of the deadly virus.
When 2019-nCoV emerged, scientists at the U.S. Centers for Disease Control and Prevention (CDC) studied the virus and its common characteristics with the former SARS (severe acute respiratory syndrome) and MERS (Middle East respiratory syndrome ) outbreaks, which are in the same virus family as the new COVID-19 coronavirus. The CDC was quick to develop its own RT-PCR test that offered the speed, sensitivity, reproducibility and reduced risk of contamination they were looking for as they faced a global concern that was expanding every day with more confirmed cases and deaths.
The CDC test was initially designed for use at the CDC only. Patient specimens from suspected cases of COVID-19 were to be sent to them for analysis and infection confirmation results while the patient in question was detained in quarantine with others awaiting their own results. But as the new virus spread to almost 30 additional countries with over 40,000 confirmed cases and approximately 1,000 deaths* (*figures as of 2-11-20), the demand for patient results became too much for the CDC to process alone.
Because of the growing amount of suspected cases that needed review, the U.S Food and Drug Administration (FDA) “issued an emergency use authorization (EUA) to enable emergency use of the Centers for Disease Control and Prevention’s (CDC) COVID-19 Real-Time RT-PCR Diagnostic Panel. Initially, this test was limited to use at CDC laboratories, but the EUA now allows the use of the test at any CDC-qualified lab across the country.”
With additional results-processing assistance throughout the country, the CDC – along with other agencies such as the FDA and the World Health Organization (WHO) – can focus on creating a vaccine and/or solution to slow down the rate of infection of the virus. With no cure available now, over 20 diagnostics companies have opted to create tests, many of them PCR-based, designed to identify virus exposure and infection in the future.
Reference:
- Digital PCR and Real-time PCR Market by Product, Application, End-user – Global Forecast to 2024. marketsandmarkets.com, October 2019. Accessed February 2020.