Beyond the bench: How artificial intelligence is redefining respiratory pathogen diagnostics in the clinical laboratory
To take the test online go HERE. For more information, visit the Continuing Education tab.
LEARNING OBJECTIVES
1. Discuss the utility for the advancement of respiratory pathogen diagnosis.
2. Discuss timelines of respiratory illnesses and the development of laboratory testing with each.
3. Define the limitations of antigen testing in the identification of respiratory pathogens.
4. Describe the different subsets of AI and each of their purposes in the use of respiratory pathogens identification.
Respiratory infections represent both a persistent and significant global health burden, necessitating accurate and timely diagnostic capabilities for effective patient management, public health interventions, and outbreak control.1 The historical trajectory of diagnostic methods for infectious diseases, particularly those affecting the respiratory system, has been a dynamic response to evolving clinical needs, consistently pushing for increased sensitivity, specificity, and speed in identifying causative agents.2 This continuous evolution underscores the pivotal role of clinical diagnostics in mitigating the impact of respiratory illnesses.
Artificial intelligence (AI) now emerges as the next frontier in the evolution of respiratory pathogen testing. It offers groundbreaking computational abilities to enhance diagnostic speed, improved accuracy, and dramatically reduced turnaround times. This signifies that AI is not merely an incremental improvement but a foundational advancement capable of bridging critical diagnostic gaps, leading to more proactive, precise clinical decision-making, and ultimately, better patient outcomes and reduced healthcare burdens.
Historical review of respiratory pathogen identification
Initial methods for respiratory illness identification relied solely on physical findings and symptoms. The Greek physician Gelan, in the first century, described symptoms of TB (tuberculosis) as night sweats, fever, and hemoptysis.3 From the mid-1800s, microbiology testing relied heavily on microscopy and cultures.4 Hans Christian Gram’s invention of the Gram stain led to significant breakthroughs in identification and classification of bacteria.5 But even then, it was not until the 1940s that Influenza cultures, using mammalian cells and or embryonated eggs, became the “gold standard” for identifying the virus.
Nearly a half century later, in 1985, Kary Mullis invented the polymerase chain reaction (PCR), ultimately leading to significant strides in the ability to identify respiratory pathogens.6 For Influenza, specifically, the advent of reverse transcriptase (RT) PCR in 1991 facilitated the detection of the virus.7 Although RT-PCR was available and in use during the 1990s and 2000s, it was not routinely used to detect respiratory pathogens. Influenza and other respiratory pathogens were primarily identified using several methods, including enzyme-linked immunosorbent assay (ELISA), immunochromatographic tests (RIDT), direct fluorescent antibody tests (DFA), and various types of cultures.8 In 2009 during the Influenza A (H1N1) Pandemic, single target PCR became the principal method for identifying respiratory pathogens in clinical laboratories.8 The H1N1 pandemic shifted the paradigm for molecular diagnostics, acting as a catalyst for clinical laboratories to adopt new technologies to better respond to the needs of their communities.
A little more than a decade later, the COVID-19 pandemic further accelerated the adoption of PCR for respiratory pathogen detection. Several US manufacturers gained Emergency Use Authorization (EUA) from the Food and Drug Administration (FDA) in 2020 for multiplex PCR tests that could detect multiple targets in a single assay, including SARS-CoV-2. The COVID-19 pandemic demonstrated how rapidly new molecular tests, especially multiplex assays, could be developed and integrated into clinical practice and with a high demand, comprehensive molecular tests became routine. Furthermore, the COVID-19 pandemic solidified the use of multiplex PCR as a common diagnostic tool, as opposed to earlier PCR assays with single targets.
While PCR was established as the new “gold standard” for respiratory pathogen identification, antigen tests also rose to prominence due to their simplicity and speed. These tests allow for the rapid identification (10–15 minutes) of the target virus, leading to quick clinical decision making. They are especially valuable during the flu and RSV (Respiratory Syncytial Virus) seasons due to their prevalent availability and ease of use. Additionally, antigen tests are significantly less expensive than their PCR counterparts and have less regulatory burden, since most tests are CLIA (Clinical Laboratory Improvement Amendments) waived.
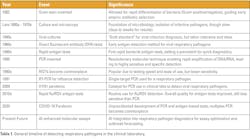
However, antigen tests have natural limitations when compared to molecular diagnostic methods. Lower levels of sensitivity make these tests less useful when patients do not display symptoms or when the viral load is below detection. For example, during the COVID-19 pandemic, the Centers for Disease Control and Prevention (CDC) recommended that repeat testing of antigen tests for SARS-CoV-2 be performed to increase diagnostic confidence because a single test could not definitively rule out an infection. Additionally, antigen tests are affected by illness onset time (when viral loads are typically peaking), specimen quality, and the prevalence of the target pathogen in the population.9 Regardless of their limitations, antigen tests still have valuable clinical utility and should be complimentary to molecular methods. See Table 1 for a summary of the timeline.
The field of respiratory pathogen diagnostics continues to rapidly evolve. Current efforts focus on further decreasing turnaround times, expanding the use of less invasive sample types (self-collected nasal swabs), and improving diagnostic stewardship to ensure appropriate test utilization.10 Future developments are likely to include the emergence of new drugs effective against a broader range of respiratory viruses, which will further justify and necessitate the extensive use of highly sensitive and specific multiplex assays to guide targeted therapies.11
The new frontier
A future development that lies beyond the bench is the integration of artificial intelligence into major segments of respiratory pathogen detection. AI is an encompassing technology with powerful subsets that transform how data is analyzed to solve complex problems. Among these, machine learning (ML), deep learning (DL), and natural language processing (NLP) stand out for their distinct capabilities and extensive application in respiratory pathogen diagnostics. While ML forms the foundational subset of AI focused on learning from data, DL represents a more advanced form utilizing multi-layered neural networks. NLP, on the other hand, empowers AI to understand and process human language.12 A summary of the subsets of AI is shown in Table 2.
Machine learning is one of the foundational subsets in the AI diaspora. It involves the creation and design of algorithms that learn from the data it analyzes. Learning is then used to automatically identify patterns and forecast outcomes while removing (or minimizing) human manipulation. In terms of respiratory pathogen diagnostics, machine learning can be effectively leveraged to predict primer specificity and sensitivity, and to optimize primer design. For example, ML can study various factors known to influence primer performance, including primer sequence, length of the primers, melting temperatures (Tm), and concentrations. By learning from datasets of successful and unsuccessful PCR reactions, ML models can distinguish complex relationships between these parameters and the outcome of the assay.13
Deep learning, a separate branch of AI that builds on ML, uses layers of neural network architecture to solve more complex and abstract problems. It does so by autonomously learning which combination of neural networks provide optimal solutions. DL offers a significant solution to accelerate RT-PCR diagnosis by applying neural networks that can predict results with a high degree of confidence. This capability is particularly useful for urgent diagnoses, where results are critical for efficient patient management and ideal allocation of hospital resources. The acceleration of RT-PCR diagnosis through deep learning has direct and significant clinical implications, especially during pandemics. By enabling an earlier prediction of results, it optimizes the utilization of critical healthcare resources (e.g., isolation rooms) and facilitates faster public health responses, demonstrating AI's capacity to enhance operational efficiency in high-pressure situations.14
A more specialized subset of AI that specializes in understanding human language is natural language processing. The major capability of NLP is taking unstructured data, such as text, notes, voice transcription, and other written forms of data, and converting it into structured data. NLP utilizes both ML and DL models to accomplish the transformation of unstructured data into structured data, which can be used to further enhance the ML and DL models it used (unsupervised, autonomous learning).15 An example of NLP advancing respiratory diagnostics would be the ability to link aspects of a patient’s electronic health record (EHR), such as history, physician notes, medical codes, and medications, into coherent and comprehensive summaries that can better inform a physician about which tests could be of value to the patient. NLP can reduce administrative cognition, allowing for more time to be spent on higher value tasks and reducing the time needed to make clinical decisions.16
Additionally, NLP can automate the interpretation of pathology and laboratory reports that are associated with PCR assays, including those used in respiratory pathogen detection. NLP models can easily analyze textual pathology reports that often accompany PCR (and other molecular methods), allowing for rapid identification of key findings, such as identified pathogens, mutations, insertions, deletions, etc.17 By automating these processes, manual review of the reports is minimized while essential information is communicated quickly.
Due to its unmatched capabilities, AI is poised to be a pivotal advancement, bridging critical diagnostic gaps that currently contribute to inappropriate treatment, suboptimal patient outcomes, and increased healthcare costs. This development suggests a profound paradigm shift from reactive, and often delayed, diagnostic processes to more proactive, precise clinical decision-making. By delivering earlier and more accurate insights, clinical laboratories can leverage AI in respiratory pathogen detection for timely interventions, potentially preventing disease progression while alleviating administrative burdens on healthcare systems.12
Concluding remarks
The trajectory of respiratory pathogen detection has significantly evolved from culture-based methods and stains to rapid antigen-based tests and progressively sophisticated molecular techniques. The advent of multiplex PCR further advanced respiratory pathogen detection by allowing for simultaneous identification of multiple pathogens from a single sample. This greatly improved efficiency and diagnostic utility. At the same time, antigen testing provides accessible, rapid, and often point-of-care solutions, crucial for quick screening and initial management, particularly during outbreaks.
Looking forward, artificial intelligence is poised to further transform respiratory pathogen detection, with clinical laboratories playing a pivotal role in leveraging AI to enhance diagnostic accuracy, optimize assay development, improve documentation, and facilitate early detection of emerging pathogens. Its successful integration will depend heavily on collaborative, interdisciplinary approaches that prioritize ethical considerations, robust validation, and continuous adaptation, ensuring that AI serves as a powerful ally in the ongoing fight against respiratory pathogens.
References
1. Esposito S, Mencacci A, Cenci E, et al. Multiplex platforms for the identification of respiratory pathogens: Are they useful in pediatric clinical practice? Front Cell Infect Microbiol. 2019;9:196. doi:10.3389/fcimb.2019.00196.
2. Vemula SV, Zhao J, Liu J, et al. Current approaches for diagnosis of influenza virus infections in humans. Viruses. 2016;8(4):96. doi:10.3390/v8040096.
3. Daniel TM. The history of tuberculosis. Respir Med. 2006;100(11):1862-70. doi:10.1016/j.rmed.2006.08.006.
4. Smith, K. How TB diagnostics have evolved since the second century. ASM.org. March 22, 2021. Accessed July 28, 2025. https://asm.org/articles/2021/march/how-tb-diagnostics-have-evolved-since-the-second-c.
5. Anekwe, L. Hans Christian Gram: The biologist who helped investigate bacteria. New Scientist. September 13, 2019. Accessed July 28, 2025. https://www.newscientist.com/article/2216418-hans-christian-gram-the-biologist-who-helped-investigate-bacteria/.
6. Khehra N, Padda IS, Swift CJ. Polymerase chain reaction (PCR). In: StatPearls. StatPearls Publishing; 2025.
7. Kumar S, Henrickson KJ. Update on influenza diagnostics: Lessons from the novel H1N1 influenza A pandemic. Clin Microbiol Rev. 2012;25(2):344-61. doi:10.1128/CMR.05016-11.
8. Patel, SN., Gubbay, JB. Impact of pandemic influenza A (H1N1) on laboratory services. National Collaborating Centre for Infectious Diseases. Published 2012. Accessed July 28, 2025. https://nccid.ca/publications/impact-of-pandemic-influenza-a-h1n1-on-laboratory-services/.
9. Testing for COVID-19. CDC. March 31, 2025. Accessed July 28, 2025. https://www.cdc.gov/covid/testing/index.html.
10. Allerton J, McKeown A. The Next Step for Respiratory Diagnostics. ID Transmission. other. February 11, 2025. Retrieved July 28, 2025, from https://www.idtransmission.com/testing/the-next-step-for-respiratory-diagnostics.
11. Esposito S, Mencacci A, Cenci E, et al. Multiplex platforms for the identification of respiratory pathogens: Are they useful in pediatric clinical practice? Front Cell Infect Microbiol. 2019;9:196. doi:10.3389/fcimb.2019.00196.
12. Dien Bard J, Prinzi AM, Larkin PMK, Peaper DR, Rhoads DD. Proceedings of the Clinical Microbiology Open 2024: Artificial intelligence applications in clinical microbiology. J Clin Microbiol. 2025;63(4):e0180424. doi:10.1128/jcm.01804-24.
13. Lee, S. Optimizing PCR primers for microbiological analysis. Number Analytics // Super Easy Data analysis tool for Research. June 10, 2025. Accessed July 28, 2025. https://www.numberanalytics.com/blog/optimizing-pcr-primers-microbiological-analysis.
14. Lee Y, Kim YS, Lee DI, et al. The application of a deep learning system developed to reduce the time for RT-PCR in COVID-19 detection. Sci Rep. 2022;12(1):1234. doi:10.1038/s41598-022-05069-2.
15. Natural language processing in healthcare medical records. ForeSee Medical. Accessed July 28, 2025. https://www.foreseemed.com/natural-language-processing-in-healthcare.
16. Clinical NLP - how to apply NLP for EHR optimization. Maruti Techlabs. Accessed July 28, 2025. https://marutitech.com/nlp-for-electronic-healthcare-record/.
17. Senders, J. T., Cote, D. J., Mehrtash, A., Wiemann, R., Gormley, W. B., Smith, T. R., Broekman, M. L., Senders JT, Cote DJ, Mehrtash A, et al. Deep learning for natural language processing of free-text pathology reports: a comparison of learning curves. BMJ Innov. 2020;6(4):192-198. doi:10.1136/bmjinnov-2019-000410.
To take the test online go HERE. For more information, visit the Continuing Education tab.
About the Author

Stephen Bishop, MBA, MS, CLS, MLS(ASCP)CM, CPHQ
MBA, MS, CLS, MLS(ASCP)CM, CPHQ
is currently the Market Director of Laboratory Services at CommonSpirit Health, Southern California. Stephen is passionate about healthcare leadership, clinical laboratory education, and process improvement.