CMV-specific immune system monitoring for management of cytomegalovirus in HSCT
Earning CEUs:
For a printable version of the January CE test go HERE or to take test online go HERE. For more information, visit the Continuing Education tab.
JANUARY LEARNING OBJECTIVES
Upon completion of this article, the reader will be able to:
1. Identify the main challenges of standard CMV treatment regimens in HSCT patients.
2. Describe the process of the immune’s response to CMV in terms of viral latency and reactivation.
3. Discuss CMV laboratory testing in HSCT patients and its limitations.
4. Discuss the physiology of the immune response to CMV in HSCT and the importance in monitoring this response in both the recipient and the donor.
Despite advances in diagnostic testing and treatment, cytomegalovirus (CMV) remains a cause of increased morbidity and mortality in allogeneic hematopoietic stem cell transplant (allo-HSCT). Anti-viral drugs are effective at reducing viral loads; yet, these drugs are expensive and have significant toxicity profiles. In general, treatment regimens are determined based on broad clinical risk stratifications, such as serostatus and haplotype matching for donor and recipient. However, a more personalized approach to risk stratification could potentially identify those individuals who may only require a reduced treatment strategy—or even no treatment strategy—thereby reducing both cost and toxicity exposure. An attractive alternative strategy consists of monitoring the patient’s CMV-specific immune response either prior to or after allo-HSCT to better inform a risk stratification strategy.1 This review will address current thinking in CMV-specific immune responses as a potential predictor of protection or susceptibility to CMV reactivation following allo-HSCT.
Viral latency
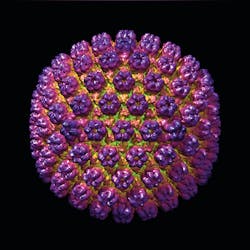
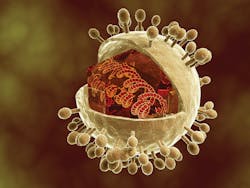
For most individuals with a healthy immune system, initial infection is either asymptomatic or is manifested by a transient period of malaise, which can present as mononucleosis or flu-like symptoms.2 During this time the virus has infected a variety of cell types, but primarily found in cells of the monocytoid lineage such as monocytes and CD34+ myeloid progenitor cells,3 where the virus persists intracellularly until changes in immune competence allows for reactivation and subsequent infection. This latency period is characterized by a homeostatic balance between viral replication and the immune response,4 and has been defined by Lemmermann et al as, “a highly dynamic condition during which episodes of viral gene desilencing, which can be viewed as incomplete reactivations, cause intermittent antigenic activity that stimulates CD8 memory-effector T cells and drives their clonal expansion. These T cells are supposed to terminate reactivation before completion of the productive viral cycle.”5
Therefore, if the infected individual remains healthy with a competent immune system, the virus will likely remain under control through immune surveillance for the life of that individual. The lifelong task of keeping the virus from uncontrolled replication results in a rise in CMV-specific T cells such as cytotoxic CD4+CD28- T cells,6 as well as CD4+CD28+ and CD8+ CMV-specific T cells. In elderly individuals, CMV-specific T cells can increase to as high as 50 percent of all CD8+ T cells and 30 percent of all CD4+ T cells.7
The delicate balance that exists between viral replication and immune system control of viral replication would suggest that a prolonged decrease in immune competence might result in a viral advantage. Loss of this balance—as seen in association with disease or drug treatment—can lead to uncontrolled viral replication resulting in CMV reactivation and disease.8 Uncontrolled viral replication can affect virtually any organ or tissue in the body and can manifest as neuropathy, pneumonia, hepatitis encephalitis, and myelitis.9 In more severe cases of immunosuppression CMV disease can present as Guillain-Barre syndrome, myocarditis, thrombocytopenia, or meningoencephalitis.10 Due to the necessity of inducing long-term immunosuppression prior to and post-transplantation, CMV reactivation, particularly for hematopoietic stem cell transplantation (HSCT), is one of the primary causes for infectious morbidity and mortality.11
CMV in HSCT
T lymphocyte ablation and immunosuppressive therapy for the HSCT recipient induces a loss of CMV-specific immunity. This loss creates a permissive environment for CMV reactivation which may approach a frequency of 70 percent when either the recipient or the donor is CMV seropositive.12 Without a prevention strategy, the majority of CMV reactivation typically occurs during the first three months after HSCT. While several antiviral drugs exist for HSCT patients, they are not routinely administered as part of a CMV prophylaxis strategy, in contrast to solid organ transplant patients. Instead, a preemptive strategy of monitoring CMV viral load is commonly used to screen for infection or reactivation. Preemptive therapy is initiated when the viral load crosses a given threshold or if a significant rate of replication of the virus is detected. Preemptive strategy success depends on the early, detectable, presence of the virus in the blood before the onset of disease.13 This usually involves frequent testing using the CMV antigenemia assay or quantitative real-time polymerase chain reaction (PCR) analysis until the likelihood of reactivation is significantly reduced, typically viewed as day 100 following transplant. While still used in some settings, antigenemia has been reported to miss up to 35 percent of PCR-positive CMV infections, and therefore a negative result may not necessarily rule out CMV infection.14
CMV nucleic acid testing (NAT), such as PCR, is one of the most common tests performed in clinical virology laboratories to identify CMV reactivation—however, there are important limitations of the test to consider. First, the viral load is simply a measure of infection; it is uninformative as to which patients may be able to—through their immune system—control infection without treatment and which patients may need treatment. Secondly, there are no validated viral load thresholds for initiation of anti-viral treatment. Universal thresholds are difficult to establish because of differences in assay platforms including, but not limited to, specimen types (blood urine, CSF, and others), blood sample preparations (whole blood, plasma, serum, and leukocytes), nucleic acid extraction methods, and targets (various CMV genes, DNA versus RNA).14 Therefore, the lack of assay standardization limits broad utility of the test results.CMV-specific immune-monitoring
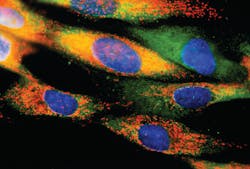
It is widely accepted that T-cell mediated cellular immunity is the most important factor in controlling CMV infection.15 Both CD4+ and CD8+ T lymphocytes are associated with protection against CMV infection with a complex interaction involving a CD8+ T cell response producing IFN-γ as well as a number of other cytokines in response to the CMV virus.16 IFN-γ has been shown to have a pivotal role in the control of CMV infection.17 A lack of CD8+ T cells in HSCT patients is associated with CMV infection, whereas immune reconstitution of CD8+ T cells is correlated with protection against CMV.18 Monitoring the patient’s CMV immune status would assist clinicians in evaluating the patient’s ability to successfully control the infection. Application of this approach may help reduce the duration and intensity of CMV monitoring, and the duration of antiviral therapy or prophylaxis in patients demonstrating a robust immune response. Alternatively, a low immune response would indicate a high likelihood of CMV reactivation and therefore indicate that continued viral monitoring or extended anti-viral treatment may be required.Importance of early immune monitoring in patients
It is generally accepted that T lymphocytes from the transplant donor are the primary source of CMV control as the recipients immunity has been ablated prior to transplant. This may be the case for fully myeloablated transplant recipients, but there is evidence that in reduced-intensity myeloablated stem cell transplants, CMV specific T cells from a seropositive recipient contribute to CMV immunity, particularly early after transplant.19 An immune response is initiated by CMV-specific T cells, primarily CMV-specific CD8 T cells, triggered by an onset of viral replication, resulting in expansion of responsive cells. Reconstitution of CMV-CD8 T cells appears to be somewhat comparable for both donor seropositive and seronegative individuals, indicating that in some cases early immune protection is conferred by recipient derived CMV-specific CD8 T cells.20 Sellar et al demonstrated that in recipient seropositive/donor seronegative (R+/D-) patients, CMV-specific CD8 T cells detected early following transplant were entirely derived by the recipient and were protective against CMV infection.20 This data indicates that recipient-derived CMV-specific CD8 T cells which had survived ablation treatment could establish a rapid reconstitution of anti-viral protection. Therefore, functional assessment of the individuals CMV-specific T cell response early, within a couple of weeks, following HSCT could provide a mechanism to establish a patient risk stratification for those likely to develop CMV infection or CMV disease, from those for whom their immune response is sufficient to provide protection. This concept has demonstrated feasibility in a study conducted by Nesher et al18 where detection of high levels of CMV-specific cells following allo-HSCT was associated with protection from CMV reactivation. While the study results are encouraging, continued research is required to fully explore the complex relationship between donor T cell reconstitution and recipient T cell survival, and how it relates to overall CMV-specific immune competence and protection against CMV reactivation.
Early identification—perhaps even prior to HCT—of patients likely to experience CMV reactivation could then be incorporated into treatment algorithms thereby helping to guide decisions on whom to treat, optimal treatment paradigms, and potentially, length of treatment. Several studies are on-going which address assessment of CMV-immune responses prior to transplant or within several weeks following transplant. It is anticipated that data from these studies will help to establish its clinical utility to risk stratify patients for personalized treatment strategies.
REFERENCES
- Yong MK, Lewin SR, Manuel O. Immune Monitoring for CMV in Transplantation. Curr Infect. Dis. Rep 2018 20:4 doi:10.1007/s11908-018-0610-4.
- Styczynski J. Who is the patient at risk of CMV recurrence: A review of the current scientific evidence with a focus on hematopoietic cell transplantation. Infect. Dis. Ther. 2018. 7:1-16. doi:10.1007/s40121-017-0180-z.
- Freer G, Quaranta P, Pistello M. Evaluation of T Cell Immunity against Human Cytomegalovirus: Impact on Patient Management and Risk Assessment of Vertical Transmission. Journal of Immunology Research. 2016;2016:9384813. doi:10.1155/2016/9384813.
- Picarda G, Benedict CA. Cytomegalovirus: Shape-Shifting the Immune System. J. Immunol. 200:3881-3889. 2018. doi:10.4049/jimmunol.1800171.
- Lemmermann NA, Böhm V, Holtappels R, Reddehase MJ. In vivo impact of cytomegalovirus evasion of CD8 T-cell immunity: facts and thoughts based on murine models. Virus Res. 2011;157(2):161–74. doi: 10.1016/j.virusres.2010.09.022.
- Broadley I, Pera A, Morrow G, Davies KA, Kern F. Expansions of Cytotoxic CD4+CD28− T Cells Drive Excess Cardiovascular Mortality in Rheumatoid Arthritis and Other Chronic Inflammatory Conditions and Are Triggered by CMV Infection. Frontiers in Immunology. 2017;8:195. doi:10.3389/fimmu.2017.00195.
- Fülöp T, Larbi A, Pawelec G. Human T Cell Aging and the Impact of
Persistent Viral Infections. Frontiers in Immunology. 2013;4:271. doi:10.3389/fimmu.2013.00271. - Sissons JG, Wills MR. How understanding immunology contributes to
managing CMV disease in immunosuppressed patients: now and in future. Med Microbiol Immunol. 2015;204: 307– 316. - Rafailidis PI, Mourtzoukou EG, Varbobitis IC, Falagas ME. Severe cytomegalovirus infection in apparently immunocompetent patients: a systematic review. Virology Journal. 2008;5:47. doi:10.1186/1743-422X-5-47.
- Blyth E, Withers B, Clancy L, Gottlieb D. CMV-specific immune reconstitution following allogeneic stem cell transplantation. Virulence, 2016;7(8), 967-980.
- Ljungman P, Hakki M, Boeckh M. Cytomegalovirus in Hematopoietic Stem Cell Transplant Recipients. Hematology/Oncology Clinics of North America. 2011;25(1):151-169. doi:10.1016/j.hoc.2010.11.011.
- Ariza-Heredia EJ, Nesher L, Chemaly RF. Cytomegalovirus diseases after hematopoietic stem cell transplantation: a mini-review. Cancer Lett. 2014;342(1):1–8. doi: 10.1016/j.canlet.2013.09.004.
- Boeckh M, Ljungman P. How we treat cytomegalovirus in hematopoietic cell transplant recipients. Blood. 2009;113(23):5711-5719. doi:10.1182/blood-2008-10-143560.
- Razonable RR, Hayden RT. Clinical Utility of Viral Load in Management of Cytomegalovirus Infection after Solid Organ Transplantation. Clinical Microbiology Reviews. 2013;26(4):703-727. doi:10.1128/CMR.00015-13.
- Boeckh M, Leisenring W, Riddell SR, et al. Late cytomegalovirus disease and mortality in recipients of allogeneic hematopoietic stem cell transplants: importance of viral load and T-cell immunity. Blood. 2003;101:407–14.
- Harari A, Zimmerli SC, Pantaleo G. Cytomegalovirus (CMV)-Specific
cellular immune responses. Hum Immunol 2004; 65:500–6. - Cummins NW, Deziel PJ, Abraham RS, Razonable RR. Deficiency of cytomegalovirus (CMV)-specific CD8+ T cells in patients presenting with late-onset CMV disease several years after transplantation. Transpl Infect Dis 2009; 11:20–7.
- Nesher L, Shah DP, Ariza-Heredia E J, et al. Utility of the enzyme-linked immunospot interferon-γ-release assay to predict the risk of cytomegalovirus infection in hematopoietic cell transplant recipients. The Journal of Infectious Diseases. 2016;213:1701–1707.
- Ogonek J, Varanasi P, Luther S, et al. Possible impact of Cytomegalovirus-specific CD8+ T cells on immune reconstitution and conversion to complete donor chimerism after allogeneic stem cell transplantation. Biol. Blood Marrow Transplant, 2017 Mar 23. pii: S1083-8791(17)30362-2. doi: 10.1016/j.bbmt.2017.03.027.
- Sellar RS, Vargas FA, Henry JY. CMV promotes recipient T-cell immunity following reduced-intensity T-cell-depleted HSCT, significantly modulating chimerism status. Blood. 2015;125:731–739.
About the Author

Ted Blanchard
MBA, serves as Senior Manager of Strategic Marketing at Oxford Immunotec USA, Inc. Blanchard has over 10 years’ experience in clinical and market development of drug and diagnostic products in the U.S. and international markets.