To take the test online go HERE. For more information, visit the Continuing Education tab.
LEARNING OBJECTIVES
Upon completion of this article, the reader will be able to:
1. Discuss healthcare statistics of various respiratory tract infections (RTIs) in the United States.
2. List the causative agents of RTIs.
3. Describe the serotypes of various viruses causing RTIs and their complications.
4. List and describe the benefits and limitations of laboratory diagnosis of RTIs.
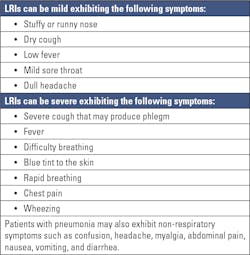
Respiratory tract infections (RTIs) are among the most common reasons why patients visit their physicians. These infections can range from mild, self-limiting, or life-threatening requiring hospitalization. Though the majority of respiratory tract infections are caused by viruses, some bacteria and fungi can also cause respiratory tract infections. RTIs can be classified as upper and lower respiratory tract infections depending on the site of the infection in the respiratory system. However, in many cases, viruses may enter the upper respiratory tract and subsequently reach the lower respiratory tract. Organisms gain entry to the respiratory tract by inhalation of droplets or contact with contaminated fomites.1,2 They then invade the mucosa, followed by epithelial destruction, along with redness, edema, hemorrhage, and sometimes an exudate.1
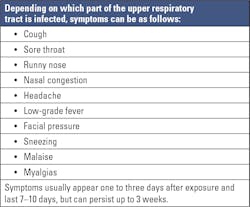
Upper respiratory tract infections (URIs) affect the respiratory tract above the lungs including the nose, throat, nasopharynx, sinus, larynx, epiglottis, or trachea causing rhinitis, pharyngitis, nasopharyngitis, sinusitis, laryngitis, epiglottitis or tracheitis respectively. They account for an estimated 10 million outpatient appointments annually.3 Though anyone can get affected by URIs, children are at a higher risk. URIs are caused by viruses in approximately 90 to 98 percent of cases.4 That said, a few bacteria and fungi can also cause URIs. Table 1 shows the probable symptoms of URIs.
Respiratory tract infections caused by viruses
Human rhinovirus and human enterovirus: Human rhinoviruses (HRVs) and respiratory enteroviruses (HEVs) are leading causes of upper respiratory tract infections and among the most frequent infectious agents in humans worldwide.8 Both are classified in the enterovirus genus within the Picornaviridae family, and they have been assigned to seven distinct species, RV-A, B, C and EV-A, B, C, D.8 HRV was first identified in the 1950s and known to cause over 50% of cases of “common cold.”9,10 The common cold is the most frequently occurring URI. Each year in the United States there are millions of cases of the common cold. Colds are the main reason that children miss school and adults miss work. Adults have an average of two to three colds per year.11 A preschool-aged child has an average of 6 to 10 episodes per year, and 10% to 15% of school-aged children have at least 12 infections per year.10 The common cold is self-limited and does not cause serious health issues. Symptoms of common cold include sore throat, runny nose, coughing, sneezing, headache, and body ache.11
Initial research suggested that HRV is a benign virus restricted to growth within the upper airways of humans. However, recent research shows that HRV is not only able to effectively reach, penetrate, and replicate within the lower airway epithelium of individuals in vivo, but also causes histologic changes of the lung interstitium and alveoli. Moreover, HRVs have now been shown to be an important cause of superinfection, with bacteria like Streptococcus pneumoniae and Staphylococcus aureus.9
Recent clinical studies in pediatrics have also shown the association of HRVs with lower respiratory tract infections including bronchiolitis and pneumonia. However, it is still not totally understood if HRVs can cause LRIs on their own. It has also been shown that both HRVs and HEVs shed in the nasopharynx of children following acute infection for up to 6 weeks and 3 weeks, respectively.12
HEV infections with non-polio enteroviruses are common in the United States during summer and fall. A mix of enteroviruses circulates every year, and different types can be common in different years.13 HEVs are found to have 4 genotypes: A, B, C, and D. Three better-known, non-polio enteroviruses are enterovirus D68 (EV-D68), enterovirus A71 (EV-A71), and coxsackie virus A6 (CV-A6). EV-D68 usually causes respiratory illness. EV-A71and CV-A6 are known to cause hand, foot, and mouth disease. Most people who get infected with non-polio enteroviruses do not get sick, or they only have mild illness, like the common cold. Symptoms of mild illness can include fever, runny nose, sneezing, cough, skin rash, mouth blisters, and body and muscle aches.13 EV-D68 can cause mild to severe respiratory illness or no symptoms at all. Mild symptoms may include runny nose, sneezing, cough, body aches, and muscle aches. Severe symptoms may include wheezing and difficulty breathing. It can also cause acute flaccid myelitis (AFM), an uncommon but serious neurologic condition that mostly affects children and causes the muscles and reflexes in the body to become weak.14
Influenza viruses: These are the next common viruses causing upper respiratory tract infection with symptoms similar to that of common cold. There are four types of influenza viruses: A, B, C, and D. Influenza A and B viruses cause seasonal flu epidemics almost every winter in the United States. Influenza A viruses are capable of causing flu pandemics. Influenza C viruses generally cause mild illness and are not thought to cause human epidemics. Influenza D viruses primarily affect cattle and are not known to infect or cause illness in people. Influenza A viruses are further divided into subtypes based on two proteins on the surface of the virus: hemagglutinin (H) and neuraminidase (N). There are 18 different hemagglutinin subtypes and 11 different neuraminidase subtypes (H1 through H18 and N1 through N11, respectively). Currently influenza A (H1N1) and influenza A (H3N2) subtypes are found in infected individuals. Influenza B viruses are not divided into subtypes, but various strains/lineages are found. Vaccines are available for influenza viruses A and B.15
The burden of influenza (flu) disease in the United States varies widely and is determined by the characteristics of circulating viruses, the timing of the season, how well the vaccine is working to protect against illness, and how many people got vaccinated. Influenza can cause mild to severe illness, and at times can lead to death.16 Flu symptoms usually come on suddenly. People who have the flu often feel some or all of these symptoms: fever, chills, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, fatigue, vomiting, and diarrhea in some, though more common in children than adults.
Most people recover in a few days to less than two weeks, but some people may develop complications. Sinus and ear infections are examples of moderate complications from flu, while pneumonia is a serious flu complication that can result from either flu virus infection alone or from co-infection of flu virus and bacteria. Other possible serious complications triggered by flu can include inflammation of the heart (myocarditis), brain (encephalitis) or muscle tissues (myositis, rhabdomyolysis), and multi-organ failure (for example, respiratory and kidney failure). Flu virus infection of the respiratory tract can trigger an extreme inflammatory response in the body and can lead to sepsis, the body’s life-threatening response to infection. The Centers for Disease Control and Prevention (CDC) estimates that flu has resulted in 9 million – 41 million illnesses, 140,000 – 710,000 hospitalizations, and 12,000 – 52,000 deaths annually between 2010 and 2020.17
Human respiratory syncytial virus (RSV): RSV is an enveloped single-stranded RNA virus of the genus Orthopneumovirus, family Pneumoviridae. It has a single serotype with two major antigenic subgroups, A and B.18 The clinical manifestations range from mild upper respiratory tract illness or otitis media to severe and potentially life-threatening lower respiratory tract involvement (LRI). The most common form of LRI in RSV-infected infants is bronchiolitis, but pneumonia and croup are also seen.18 Most people recover in a week or two, but it can also be serious, especially for infants and older adults. It is the most common cause of bronchiolitis and pneumonia in children younger than one year of age in the United States.19
Human coronavirus and SARS-CoV-2: There are six human pathogenic coronaviruses (CoV) that primarily cause respiratory infections in humans. Four of them, 229E (alpha coronavirus), NL63 (alpha coronavirus), OC43 (beta coronavirus), and HKU1 (beta coronavirus) occur worldwide and are very common. These viruses usually cause mild to moderate upper respiratory tract infections after 2–10 days of incubation with the typical symptoms of a cold or flu-like infection, i.e., runny nose, cough, sore throat, headache, and fever or feverishness. Severe cases are rare and are most likely to occur in immunosuppressed patients. Two other types are rare but responsible for severe viral pneumonia: MERS (Middle East respiratory syndrome) and SARS-CoV (severe acute respiratory syndrome). While SARS-CoV has not been found in humans since 2004, infections with MERS-CoV have been continuously detected since 2012.20
SARS-CoV-2 is a coronavirus discovered in 2019 that caused the COVID-19 pandemic. Per World Health Organization (WHO) data, as of December 13, 2022, it caused 652 million cases with 6.6 million deaths worldwide and 99.6 million cases with 1.1 million deaths in the United States.21 The virus keeps mutating resulting in eight variants so far — Alpha, Beta, Gamma, Delta, Omicron, Lambda, Mu, and BA.2. The virus spreads mainly from person to person through respiratory droplets produced when an infected person coughs, sneezes, or talks. Some people who are infected may not have symptoms. For people who have symptoms, illness can range from mild to severe. Adults 65 years and older and people of any age with underlying medical conditions are at higher risk for severe illness.22 Main symptoms are fever, cough, shortness of breath, trouble breathing, fatigue, chills, body aches, headache, sore throat, congestion/runny nose, loss of smell or taste, nausea, diarrhea. The virus can lead to pneumonia, respiratory failure, heart problems, liver problems, septic shock, and death.23
Human adenovirus: A DNA virus that most commonly causes respiratory illness. The illnesses can range from the common cold to pneumonia, croup, and bronchitis. People with weakened immune systems are at high risk for developing severe illness caused by adenovirus infection.24
Human parainfluenza viruses (HPIV): Commonly cause respiratory infections in infants and young children. Patients usually recover on their own. However, HPIVs can also cause more severe illness, such as croup or pneumonia.25
Human metapneumovirus (HMPV): Can cause upper and lower respiratory disease in people of all ages, especially among young children, older adults, and people with weakened immune systems. Symptoms commonly associated with HMPV include cough, fever, nasal congestion, and shortness of breath. Clinical symptoms of HMPV infection may progress to bronchitis or pneumonia.26
Human bocavirus (HBoV1): Small, nonenveloped linear single-stranded DNA virus of the Parvoviridae family that was discovered in 2005 in nasopharyngeal aspirates of children with respiratory tract infections. HBoV1 causes both upper and lower respiratory tract infections of diverse severity and affects most children before age seven. After primary infection, HBoV1 can, despite a vigorous antibody response, persist in the respiratory tract for at least up to 12 months.27
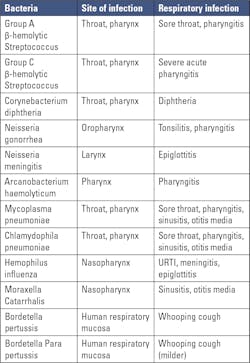
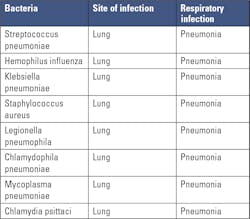
Respiratory tract infections caused by bacteria
Though viruses are known to cause more cases of respiratory tract infections, some bacteria can cause upper and lower respiratory tract infections.1 Co-infection with a virus and bacteria may contribute to severe disease and increased mortality in patients.28Table 3 lists the common bacteria causing upper respiratory tract infections and Table 4 lists the bacteria that cause lower respiratory tract infections, mostly pneumonia.Laboratory diagnosis of respiratory viruses and bacteria
Proper diagnosis to determine the causative organism is very important for proper patient management. There are several methods for detecting and identifying respiratory viruses and bacteria and every method has its pros and cons, which are listed below.29
Electron microscopy: Though electron microscopy had been used in the past to identify novel viral strains, its use is limited in diagnosis as it is expensive, laborious, time-consuming, and is not as sensitive compared to many other diagnostic methods.
Culture: Culture has been considered the gold standard for both viruses and bacteria for decades. There have been several improvements in the viral culture process over time. That said, some viruses, including rhinovirus and coronavirus, are difficult to grow and repeated freeze thaw of samples can lower the viral titer affecting growth of the viral culture.
Viral cultures are time consuming, laborious, and can result in false negatives. Bacterial cultures are easier to grow, but testing takes 48 to 96 hours when the culture is followed by drug susceptibility testing. Also, if the sample is collected after antimicrobial treatment, false negative results may be seen.
Rapid immunoassays: Rapid immunoassays (RIAs) can deliver test results in less than 30 minutes even when the patient is at the doctor’s office, enabling early patient management and treatment. Knowing the causative agent early helps to check spread of the disease. RIAs are relatively inexpensive, easy to perform, and most are CLIA-waived, thereby making them invaluable in outpatient, primary care, emergency, and low-resource settings. In spite of these benefits, RIA tests vary greatly in sensitivity, and RIA may not be available for all types of respiratory viruses and bacteria.
Direct fluorescent antibody tests: Direct fluorescent antibody (DFA) testing of nasopharyngeal wash specimens is considered a rapid and reliable method for detecting respiratory viral infections. Many commercial DFA kits have high sensitivity and specificity, but the results can be subjective and require technical expertise for accurate interpretation.
Serological tests: Pathogen-specific antibodies generally appear about two weeks after the initial infection and can be detected by serological tests. Serological tests can successfully identify antibodies to most respiratory pathogens such as RSV, adenovirus, influenza A and B, parainfluenza 1-3 virus, etc. These tests can also detect mixed infections from hospitalized children suffering from acute respiratory infections. That said, antibody response in infants is not well detected and serological tests against all viruses and bacteria may not be very sensitive.
Nucleic acid amplification tests: A wide variety of nucleic acid amplification tests (NAATs) for the detection of respiratory pathogens are commercially available. NAAT tests are highly specific and have high sensitivity. However, they are generally more expensive than immunoassays and some require high technical skill. The tests are of varying complexity, including:
- Rapid, CLIA-waived tests that detects one or a few pathogens
- Moderately complex test that detects a few pathogens
- Highly complex multiplex assays detecting several pathogens simultaneously
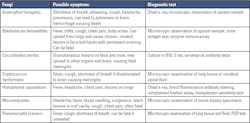
Respiratory tract infections caused by fungi
Respiratory tract infections caused by fungi have been reported in immunocompromised patients. Table 5 lists some fungi that cause respiratory infections, along with symptoms and diagnostic tests.30
Conclusion
As respiratory tract infections exhibiting similar symptoms may be caused by different pathogens with varying prognosis, it is necessary to accurately identify the causative pathogen at the earliest point possible.
Benefits of early detection and initiation of appropriate patient management are as follows:
- Rapid recovery of the patient;
- Check transmission of the infectious agent especially in case of highly infectious viruses;
- Curtail unnecessary use of antibiotics and prevent antibiotic resistance when the infection is found to be of viral origin, as antibiotics are known to be ineffective against viruses.
REFERENCES
1. Dasaraju PV, Liu C. Infections of the Respiratory System. In: Baron S, editor. Medical Microbiology. 4th edition. Galveston (TX): University of Texas Medical Branch at Galveston; 1996. Chapter 93. Available from: https://www.ncbi.nlm.nih.gov/books/NBK8142/.
2. Charlton CL, Babady E, Ginocchio CC, Hatchette TF, et al. Practical Guidance for Clinical Microbiology Laboratories: Viruses Causing Acute Respiratory Tract Infections. Clin Microbiol Rev. 2018;12;32(1):e00042-18. doi:10.1128/CMR.00042-18.
3. Thomas M, Bomar PA. Upper Respiratory Tract Infection. [Updated 2022 Jun 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532961/.
4. Chow AW, Benninger MS, Brook I, et al. IDSA clinical practice guideline for acute bacterial rhinosinusitis in children and adults. Clin Infect Dis. 2012;54(8):e72-e112. doi:10.1093/cid/cir1043.
5. GBD 2019 LRI Collaborators. Age-sex differences in the global burden of lower respiratory infections and risk factors, 1990-2019: results from the Global Burden of Disease Study 2019. Lancet Infect Dis. 2022;22(11):1626-1647. doi:10.1016/S1473-3099(22)00510-2.
6. Chowdhary A, Agarwal K, Meis JF. Filamentous Fungi in Respiratory Infections. What Lies Beyond Aspergillosis and Mucormycosis? PLoS Pathog. 2016;28;12(4):e1005491. doi:10.1371/journal.ppat.1005491.
7. Fletcher J. Lower respiratory tract infection: Symptoms, diagnosis, and treatment. Medicalnewstoday.com. Published February 11, 2019. Accessed December 20, 2022. https://www.medicalnewstoday.com/articles/324413.
8. Royston L, Tapparel C. Rhinoviruses and Respiratory Enteroviruses: Not as Simple as ABC. Viruses. 2016; 11;8(1):16. doi:10.3390/v8010016.
9. Smith ME, Wilson PT. Human Rhinovirus/Enterovirus in Pediatric Acute Respiratory Distress Syndrome. J Pediatr Intensive Care. 2020;9(2):81-86. doi:10.1055/s-0039-3400466.
10. Loo M. Upper Respiratory Tract Infection. Integrative Medicine for Children. Published online 2009:450-455.
11. CDC. Common colds: Protect yourself and others. Centers for Disease Control and Prevention. Published November 29, 2021. Accessed December 20, 2022. https://www.cdc.gov/features/rhinoviruses/index.html.
12. Jartti T, Lehtinen P, Vuorinen T, Koskenvuo M, Ruuskanen O. Persistence of rhinovirus and enterovirus RNA after acute respiratory illness in children. J Med Virol. 2004;72(4):695-9. doi:10.1002/jmv.20027.
13. CDC. Enteroviruses. Centers for Disease Control and Prevention. Published November 14, 2022. Accessed December 22, 2022. https://www.cdc.gov/dotw/enteroviruses/index.html.
14. Enterovirus D68. Cdc.gov. Published September 9, 2022. Accessed December 22, 2022. https://www.cdc.gov/non-polio-enterovirus/about/ev-d68.html.
15. CDC. Types of influenza viruses. Centers for Disease Control and Prevention. Published December 2, 2022. Accessed December 22, 2022. https://www.cdc.gov/flu/about/viruses/types.htm.
16. CDC. Flu symptoms & complications. Centers for Disease Control and Prevention. Published November 30, 2022. Accessed December 22, 2022. https://www.cdc.gov/flu/symptoms/symptoms.htm.
17. CDC. Disease burden of flu. Centers for Disease Control and Prevention. Published December 1, 2022. Accessed December 22, 2022. https://www.cdc.gov/flu/about/burden/index.html.
18. Borchers AT, Chang C, Gershwin ME, Gershwin LJ. Respiratory syncytial virus--a comprehensive review. Clin Rev Allergy Immunol. 2013;45(3):331-79. doi:10.1007/s12016-013-8368-9.
19. CDC. Learn about respiratory syncytial virus infection (RSV). Centers for Disease Control and Prevention. Published November 9, 2022. Accessed December 22, 2022. https://www.cdc.gov/rsv/index.html.
20. Corman VM, Lienau J, Witzenrath M. Coronaviren als Ursache respiratorischer Infektionen [Coronaviruses as the cause of respiratory infections]. Internist (Berl). 2019;60(11):1136-1145. German. doi:10.1007/s00108-019-00671-5.
21. WHO Coronavirus (COVID-19) dashboard. Who.int. Accessed December 22, 2022. https://covid19.who.int/.
22. CDC. Coronavirus disease 2019 (COVID-19). Centers for Disease Control and Prevention. Published December 19, 2022. Accessed December 22, 2022. https://www.cdc.gov/dotw/covid-19/index.html.
23. Coronavirus (COVID-19) overview. WebMD. Accessed December 22, 2022. https://www.webmd.com/covid/coronavirus.
24. Clinical overview. Cdc.gov. Published November 23, 2022. Accessed December 22, 2022. https://www.cdc.gov/adenovirus/hcp/clinical-overview.html.
25. Human Parainfluenza viruses (HPIVs). Cdc.gov. Published November 18, 2022. Accessed December 22, 2022. https://www.cdc.gov/parainfluenza/index.html.
26. Human metapneumovirus clinical features - NREVSS. Cdc.gov. Published November 29, 2022. Accessed December 22, 2022. https://www.cdc.gov/surveillance/nrevss/hmpv/clinical.html.
27. Xu M, Perdomo MF, Mattola S, et al. Persistence of Human Bocavirus 1 in tonsillar germinal centers and antibody-dependent enhancement of infection. MBio. 2021;12(1). doi:10.1128/mBio.03132-20.
28. Liu Y, Ling L, Wong SH, Wang MH, et al. Outcomes of respiratory viral-bacterial co-infection in adult hospitalized patients. EClinicalMedicine. 2021;10;37:100955. doi:10.1016/j.eclinm.2021.100955.
29. Das S, Dunbar S, Tang YW. Laboratory diagnosis of respiratory tract infections in children - the state of the art. Front Microbiol. 2018;9:2478. doi:10.3389/fmicb.2018.02478.
30. Fungal Infections of the Respiratory Tract: Geoff’s Essential Microbiology. 2019.